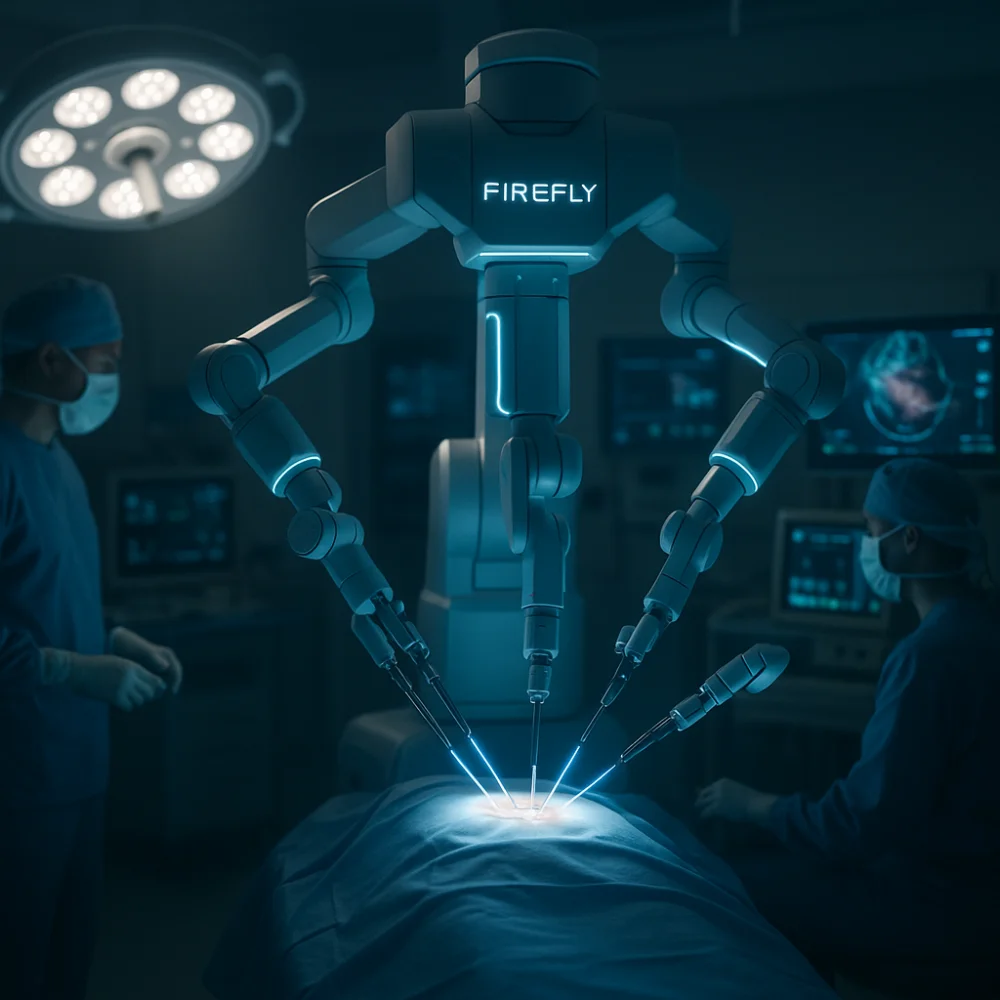
Firefly fluorescence imaging revolutionizes surgical procedures by providing real-time visualization of tissue perfusion and vascular structures through near-infrared technology. The system enables surgeons to distinguish between healthy vascularized tissue and compromised areas with 83% accuracy in tumor detection. Its seamless integration with robotic surgical systems eliminates equipment repositioning while offering 3D magnified views of critical vessels and anatomical boundaries. This advancement significantly reduces inadvertent injuries and enhances precision across multiple surgical specialties, alters minimally invasive procedural outcomes.
Advanced fluorescence imaging represents a change in approach in surgical visualization, fundamentally altering how surgeons differentiate between tissue types during complex procedures. This technology employs near-infrared fluorescence to provide real-time visualization of anatomical structures through indocyanine green dye, which fluoresces bright green under infrared light. The system enables clear differentiation between vascularized healthy tissue and non-vascularized or tumor-affected areas based on distinct fluorescence patterns.
Integrated directly into robotic platforms like da Vinci XI, this technology offers magnified 3D imaging of microperfusion and tissue contours. The technology proves particularly valuable in ureteral reconstruction procedures where previous surgeries have created challenging fibrotic environments that obscure normal anatomical landmarks. Molecular imaging techniques using targeted fluorescent antibodies enhance tumor detection capabilities, while fluorescent dye optimization allows multiple administration modes. Studies demonstrate 83% concordance between decreased fluorescence and tumor presence, significantly improving intraoperative localization accuracy compared to traditional visual methods.
Firefly technology’s real-time vascular mapping capabilities enable surgeons to track live blood flow patterns throughout surgical procedures, providing continuous visualization of perfusion status in target tissues. This active imaging approach protects indispensable structures by clearly delineating critical vessels and their anatomical relationships, significantly reducing the risk of inadvertent injury during complex dissections. The immediate visual feedback enhances intraoperative decision-making by allowing surgeons to adjust their surgical approach based on real-time vascular assessments rather than relying solely on preoperative imaging data. The technology utilizes specialized dye injections that highlight tissue characteristics, enabling surgeons to distinguish between different tissue types with enhanced precision during the procedure.
Real-time vascular mapping represents one of the most significant breakthroughs in modern surgical guidance, enabling surgeons to visualize blood flow patterns and anatomical structures with unparalleled clarity during complex procedures. Through indocyanine green dye administration, Firefly technology illuminates vascular networks using near-infrared fluorescence imaging, providing immediate feedback on tissue perfusion status. This precise anatomical mapping capability allows surgeons to distinguish between healthy and compromised tissues while maintaining optimal blood supply throughout operations.
The technology’s intraoperative organ preservation benefits are particularly evident in cancer surgeries, where surgeons can differentiate malignant from benign tissues with enhanced accuracy. By offering detailed blood flow visualization, Firefly enables safer traversal through complex surgical sites, reducing complications and facilitating efficient dissection while protecting crucial structures from inadvertent damage. The device’s portable design makes it accessible across various surgical environments, ensuring consistent recovery monitoring capabilities during extended procedures.
The ability to visualize blood flow patterns during surgery extends beyond tissue assessment to provide surgeons with unparalleled protection capabilities for essential anatomical structures. Firefly technology’s real-time vascular mapping enables precise anatomical boundaries recognition, allowing surgeons to distinguish between healthy tissue and scarred areas from previous operations. This enhanced visualization proves particularly helpful when normal surgical planes are disrupted, helping surgeons navigate complex anatomical terrain safely.
The system’s integration with robotic platforms delivers instant switching between fluorescence and standard views, maintaining surgical workflow while protecting indispensable structures. Critical structure preservation becomes significantly more achievable as surgeons can identify small but critical vessels and neural pathways that might otherwise remain hidden. This technology reduces inadvertent injuries to arteries, veins, and other delicate tissues during complex reconstructive procedures. In gynecologic surgery specifically, the combination of NIRF and transillumination provides clear anatomical landmarks that enhance surgical precision during procedures such as hysterectomies and bladder endometriosis resections.
During critical surgical moments, surgeons must make split-second decisions that can determine patient outcomes, and Firefly technology’s near-infrared fluorescence imaging modifies these high-stakes choices by providing instantaneous vascular perfusion data directly to the operating field. The system’s real-time blood flow mapping enables perceptive assessment of tissue viability, allowing surgeons to identify microvascular obstructions invisible on standard imaging. This surgical flow optimization prevents unnecessary tissue removal while ensuring adequate perfusion margins. When combined with robotic platforms like the da Vinci XI system, surgeons receive intraoperative guidance information through seamless toggling between normal and fluorescence views. The enhanced visualization capability reduces intraoperative errors and supports evidence-based decisions during complex procedures, ultimately improving patient safety and surgical outcomes.
Advanced fluorescence imaging capabilities modify surgical precision through Firefly technology’s embedded integration within da Vinci robotic systems. The seamless incorporation allows surgeons to toggle between normal white light and near-infrared fluorescence imaging without interrupting their workflow. This system integration efficiency eliminates the need for additional equipment or repositioning during procedures.
Firefly employs indocyanine green dye as a contrast agent, captured by specialized cameras integrated into the da Vinci endoscope. Surgeons access fluorescence imaging directly from the console interface, enabling real-time tissue perfusion analysis. The technology combines with 3D magnified views to enhance image guidance capabilities for complex minimally invasive surgeries.
This workflow optimization maintains continuous surgical flow while providing enhanced visualization of blood vessels, tissue viability, and anatomical structures that may be difficult to distinguish under conventional lighting conditions.
The integration of Firefly fluorescence imaging with robotic surgical platforms has demonstrated measurable improvements in patient outcomes across multiple clinical parameters. Studies consistently report significant reductions in intraoperative blood loss and lower rates of major complications, including decreased incidences of ureteral and bowel injuries during complex procedures. Additionally, the enhanced visualization capabilities contribute to improved oncological outcomes through more thorough lymph node retrieval and complete tumor resection rates.
One of the most significant clinical advantages of Firefly robotic technology lies in its ability to dramatically reduce intraoperative blood loss across varied surgical procedures. Clinical evidence demonstrates substantial reductions, with gastrectomy patients experiencing 30.7 mL versus 73.3 mL blood loss compared to conventional approaches. The technology’s real-time near-infrared fluorescence enables precise visualization of blood vessels and anatomical structures, allowing surgeons to perform more accurate dissections while avoiding unnecessary vascular injury. Enhanced three-dimensional imaging and tremor filtration contribute to superior procedural safety enhancement by minimizing inadvertent tissue damage. Additionally, reduced operative time through Firefly guidance limits cumulative bleeding exposure. This blood conservation translates into decreased transfusion requirements, faster recovery periods, and improved overall patient outcomes across oncologic and complex surgical interventions.
Beyond reducing blood loss, Firefly robotic technology exhibits exceptional efficacy in lowering overall complication rates across varied surgical procedures. The fluorescence imaging system enables precise tissue perfusion assessment, preventing ischemic complications through accurate identification of viable versus nonviable tissue. This enhanced visualization significantly reduces anastomotic leak rates and ureteral injuries during complex reconstructive surgeries.
| Complication Type | Traditional Surgery | Firefly-Assisted Surgery |
| Anastomotic Leaks | 3-8% | 0.4-1.5% |
| Ureteral Injury | 2-5% | <1% |
| Stricture Recurrence | 15-25% | 5-10% |
The technology’s real-time guidance facilitates improved surgical workflow by minimizing intraoperative errors and reducing collateral tissue damage. Consequently, patients experience reduced recovery time due to fewer postoperative complications, shorter hospital stays, and decreased need for secondary interventions.
Several pioneering applications distinguish Firefly robotic technology’s impact on cancer treatment, fundamentally altering how surgeons approach oncologic procedures. Near-infrared fluorescence imaging with indocyanine green dye enables real-time visualization of cancerous tissues and tumor boundaries during surgery. This enhanced visualization facilitates improved surgical margins by accurately identifying malignant tissue, ensuring complete removal while preserving healthy structures. The technology eliminates uncertainties associated with conventional marking methods, reducing ink scattering and enhancing lesion detection accuracy.
Firefly’s precision significantly contributes to reduced recurrence risk by minimizing residual cancer cells through adequate resection margins. The system proves particularly precious in challenging cancers like rectal and endometrial cases, where precise tumor localization is critical for optimal outcomes and long-term cancer control.
Firefly robotics technology has exhibited exceptional versatility across multifarious surgical specialties, profoundly altering how surgeons perceive and maneuver intricate anatomical structures. The system’s near-infrared fluorescence imaging enables precise endocrine gland identification during thyroid procedures while facilitating comprehensive tissue viability assessment across reconstructive surgeries.
| Specialty | Primary Application | Key Benefit |
| Urology | Microvascular perfusion visualization | Reduced stricture rates |
| Gynecology | Lymph node identification | Enhanced surgical precision |
| Colorectal | Anastomotic blood supply assessment | Decreased complications |
This technological advancement transforms surgical workflows by providing real-time anatomical guidance, enabling surgeons to preserve healthy tissue while achieving optimal therapeutic outcomes. The integration facilitates minimally invasive approaches, replacing traditional open procedures and significantly improving patient recovery trajectories across assorted surgical disciplines.
While the versatility of firefly robotics spans numerous surgical disciplines, its most revolutionary effect manifests in oncological procedures where precision dictates patient survival outcomes. Near-infrared fluorescence imaging transforms tumor visualization by using indocyanine green dye to clearly delineate cancerous tissue from surrounding structures. This enhanced visualization enables surgeons to achieve optimal oncological margins preservation while maximizing healthy tissue preservation during complex resections.
The technology proves particularly crucial in partial nephrectomies and gynecologic cancers, where precise tumor boundaries determine surgical success. Real-time vascular perfusion assessment allows surgeons to preserve viable tissues while ensuring complete tumor removal. This precision reduces incomplete resections, minimizes unnecessary tissue excision, and enables organ-sparing approaches that maintain postoperative function while achieving superior oncologic outcomes.
The integration of firefly robotics with minimally invasive surgical platforms represents a shift that fundamentally expands the boundaries of what surgeons can accomplish through small incisions. Real-time near-infrared fluorescence imaging enables complex anatomical reconstruction previously considered too challenging for minimally invasive approaches. Surgeons can now perform intricate ureteral repairs, bladder reconstructions, and gynecologic procedures with unparalleled precision through robotic systems.
The technology eliminates traditional barriers by providing fluid vascular mapping and tissue perfusion assessment during surgery. Studies demonstrate zero intraoperative complications and shorter recovery times, with patients averaging 5.9-day hospital stays. This advancement transforms minimally invasive revision surgeries, particularly in cases involving scar tissue or distorted anatomy where conventional visualization fails, ultimately expanding surgical options across multiple specialties.
Surgical robotics markets are experiencing unparalleled expansion, with global valuations projected to surge from USD 6.2 billion in 2022 to approximately USD 25.7 billion by 2032, representing a compound annual growth rate of 15.7%. This rapid globalization reflects substantial investment momentum, evidenced by North America’s 8.8% robot sales growth in Q3 2024, generating $475 million revenue. Emerging markets demonstrate extraordinary potential, with India’s installations surging 59% in 2023 due to expanding healthcare infrastructure.
Technological developments amplify adoption prospects through generative AI integration, projected to reach $98.1 billion by 2025 with 36.5% CAGR growth. Advanced AI capabilities enhance surgical precision through computer vision and real-time decision support systems. Government funding supports innovation, with US allocating $1.2 billion toward AI research, while venture capital investments signal sustained confidence in surgical robotics evolution.
At Dr. Brian Harkins, we believe Firefly robotics represents a revolutionary advancement in surgical technology that is fundamentally changing how surgeons visualize and perform complex procedures. By combining enhanced fluorescence imaging with real-time vascular mapping, our Firefly-enabled systems improve surgical precision and help reduce patient complications. Designed for seamless integration with existing robotic platforms, Firefly robotics from Dr. Brian Harkins is already proving versatile across multiple specialties and clinical applications. As adoption grows and we continue to advance the technology, Dr. Brian Harkins is committed to establishing Firefly robotics as an essential tool for modern minimally invasive surgery.
Robotic surgery builds upon the foundation of laparoscopic surgery by adding robotic arms that offer advanced surgical precision and 3D magnified visualization. While laparoscopy relies on rigid instruments and manual dexterity, robotic systems like the da Vinci surgical system provide robotic precision that greatly improves accuracy in delicate procedures, lowering the conversion rate to open surgery and enhancing overall surgical care.
In urologic surgery, robotic-assisted surgery has become a gold standard, particularly for prostate and kidney operations. Looking ahead, future directions focus on personalized surgery and the integration of AI in robotic systems to refine optimized surgical approaches. This will allow robotic platforms to adapt in real time, personalizing surgical approaches and reducing complications while enhancing patient-centered surgical care.
A robotic surgeon controls the da Vinci surgical console, where hand movements translate into scaled, tremor-free motions of the robotic arms. This technology gives the surgeon unmatched control in the surgical field, enabling them to perform surgery with precision that surpasses traditional methods. This system is especially valuable for minimally invasive robotic surgery where enhances the precision of complex dissections.
Research and development drives constant innovation, fueling advancements in robotic platforms. From surgical techniques in minimally invasive colorectal surgery to robotic pancreatic surgery, ongoing research and systematic review and meta-analysis continue to demonstrate that robotic surgery holds immense promise. New prototypes like the ARTAS system and another autonomous system are examples of how subsequent advancements led to broader surgical applications across specialties.
Robotic-assisted surgery offers reduced blood loss, smaller incisions, and faster recovery compared to open surgery. Particularly in urologic robotic and minimally invasive colorectal surgery, it provides advanced surgical outcomes with lower complication risks. However, despite these benefits, surgery is a rapidly evolving field, and a review of the literature highlights that despite these advancements, cost and accessibility remain challenges.
The integration of artificial intelligence into surgical systems represents a paradigm shift. AI into robotic surgery holds potential for personalizing surgical approaches, predicting complications, and enabling artificial intelligence in medicine to become routine in surgical settings. Integrating artificial intelligence ensures improved surgical training, while discussions on AI and ethics are crucial to ensure responsible deployment.
Surgery using Firefly introduces near-infrared fluorescence that makes blood vessels and tissue perfusion visible. When used during robotic surgery, it allows surgeons to identify critical structures with clarity, particularly in delicate procedures. This integration into the da Vinci surgical system supports advanced surgical precision and contributes to personalized surgery by preserving healthy tissues in particularly in complex oncologic cases.
Innovations in surgical robotics extend beyond general procedures into specialized areas such as complex brain surgery, robotic low ligation in colorectal cases, and robotic pancreatic surgery. Each of these surgical subspecialties benefits from advanced surgical precision and optimized surgical approaches, which not only improve outcomes but also lead to improved surgical training for the next generation of surgeons.
A systematic review and meta-analysis consistently demonstrates that robotic surgery is a rapidly expanding field with superior short-term outcomes compared to traditional methods. Reduced conversion rate to open surgery, shorter recovery times, and fewer complications are common themes in every review of the literature, reinforcing the idea that artificial intelligence surgery and robotic integration are transforming surgical applications across specialties.
The advent of robotic systems like the da Vinci system and emerging another autonomous system emphasizes patient-centered surgical care. These technologies allow for personalized surgery, faster recovery, and safer outcomes across surgical settings. With AI has the potential to enhance decision-making and workflow, the role of artificial intelligence will be critical in ensuring that artificial intelligence surgery remains ethical, effective, and beneficial for all patients.


Dr. Brian Harkins is a renowned surgeon specializing in advanced, minimally invasive, and robotic surgical techniques. With a dedication to innovation and personalized patient care, he has transformed countless lives by delivering exceptional outcomes.

I want a website like this, where do i start?