
Firefly imaging technology offers surgeons real-time fluorescent visualization using dyes like indocyanine green to distinguish healthy tissue from cancerous areas. This advanced system enables precise tumor margin detection, reducing cancer recurrence risk through complete resection. The technology enhances blood flow assessment within 30-60 seconds, confirming tissue viability and vascular patency. It integrates seamlessly with robotic surgical platforms, supporting minimally invasive procedures across urology, gynecology, and oncology specialties while improving patient outcomes and reducing complications. Further exploration reveals additional groundbreaking surgical applications.
How does firefly imaging enable surgeons to distinguish cancerous tissue from healthy tissue during live surgical procedures? The technology employs fluorescent dyes like indocyanine green (ICG) injected intravenously or locally to create distinct visual contrasts. Under near-infrared light, healthy tissue fluoresces bright green while cancerous tissue remains dark, providing clear differentiation. This tissue characterization enhancement allows surgeons to identify exact tumor margins and track vascular supply in real-time. Multi-wavelength fluorescence imaging enables simultaneous differentiation of multiple tissue types, supporting all-encompassing intraoperative assessment. The technology’s ability to highlight tissue vascularization and perfusion patterns further aids in distinguishing healthy from unhealthy tissue. This precise visualization contributes to intraoperative risk reduction by helping surgeons avoid critical structures while ensuring complete tumor removal without leaving residual cancerous tissue behind. The technology enables surgeons to perform minimally invasive surgery while preserving maximum healthy organ tissue, reducing the need for complete organ removal.
While traditional surgical approaches rely on delayed histopathologic assessment to determine margin adequacy, firefly imaging revolutionizes cancer surgery by enabling real-time, precise tumor margin detection that significantly reduces the risk of cancer recurrence. By achieving negative surgical margins (R0) through fluorescence guidance, surgeons minimize residual malignant cells that could trigger local recurrence. The technology’s ability to detect microscopic tumor deposits intraoperatively prevents microscopic residual disease, a primary cause of cancer relapse. Multiple clinical studies demonstrate increased complete tumor resection rates with fluorescence-guided surgery, correlating with improved postoperative outcomes. This immediate margin feedback enables repeated intraoperative checks and facilitates optimized surgical workflow by eliminating dependence on delayed pathology results while ensuring exhaustive tumor removal. The fluorescence detection system utilizes DyLight 800 conjugated antibodies to provide enhanced imaging capabilities for tumor visualization.
Beyond identifying tumor margins, firefly imaging alters surgical decision-making through its capacity to provide instantaneous blood flow and tissue perfusion assessment. This technology enables real-time visualization of circulation within 30-60 seconds of indocyanine green injection, allowing surgeons to confirm vascular graft patency and assess organ viability during procedures. Intraoperative tissue evaluation becomes objective rather than subjective, as surgeons can differentiate perfused regions from ischemic areas with precision. Microvascular blood flow monitoring proves particularly beneficial in minimally invasive surgeries where tactile feedback is limited. The system supports selective arterial clamping decisions, guides tissue preservation strategies, and prevents postoperative complications like ischemic gastropathy by ensuring adequate blood supply before surgical closure. In robotic cardiac procedures, the technology compensates for the lack of tactile feedback by providing visual confirmation of vessel integrity and graft quality during harvest and anastomosis.
Firefly imaging technology seamlessly integrates with modern robotic surgical platforms, most notably the da Vinci Surgical System, altering the scenery of minimally invasive procedures. This integration enables real-time fluorescence visualization without disrupting seamless surgical workflow, allowing surgeons to maintain complete control through the robotic console’s 3D magnified view. When indocyanine green dye is administered, vascular structures and tissue perfusion appear distinctly in fluorescence mode, providing precise anatomical delineation of critical structures. The technology combines white light endoscopy with fluorescence imaging in one unified platform, eliminating the need for separate equipment or workflow interruptions. This advancement greatly improves the capabilities of robotic systems, making them exceptionally well-suited for complex minimally invasive surgeries while improving surgical precision and patient outcomes. The enhanced visualization capabilities are particularly valuable for urinary tract reconstruction, where precise identification of anatomical structures is critical for successful outcomes.
Firefly imaging technology has demonstrated extraordinary versatility across multiple surgical specialties, with particularly significant applications in urology and gynecology. In urological procedures, the technology enables precise tumor identification during renal resections and supports complex reconstructive surgeries through enhanced visualization of anatomical structures. Gynecologic surgeons employ Firefly imaging for sentinel lymph node mapping and endometriosis lesion identification, while oncologic applications across specialties benefit from improved tumor margin delineation and real-time assessment of tissue perfusion.
Surgical precision in urology and gynecology has been significantly enhanced through the integration of firefly imaging technology, which provides real-time visualization of vascular anatomy and tissue perfusion during complex procedures. In urological applications, the technology enables reconstructive procedure enhancement through improved microperfusion visualization in 3D magnified fields. Surgeons can safely identify ureters embedded in fibrotic tissue while performing selective clamping during partial nephrectomy, reducing warm ischemia time by approximately two minutes without compromising outcomes.
Gynecologic surgery benefits from enhanced endometriosis lesion visualization through abnormal vascular proliferation illumination. The technology assists in delineating anatomical landmarks during hysterectomies and pelvic lymphadenectomy, while improving colpotomy border identification. This intraoperative vascular anatomy visualization reduces complications and conversion rates, ultimately shortening recovery times through improved tissue preservation.
Beyond reproductive and urinary tract procedures, oncologic surgery represents one of the most impactful applications of firefly imaging technology, where precision directly correlates with patient survival outcomes. The technology enables improved accuracy of tumor resection margins through real-time visualization, reducing local recurrence rates and enhancing overall survival. Fluorescent guidance minimizes residual tumor burden while protecting essential structures during complex dissections.
Firefly imaging demonstrates increased precision of lymph node mapping, particularly in sentinel lymph node identification for various cancers. ICG dye highlights lymphatic channels under near-infrared imaging, improving detection accuracy while reducing unnecessary node removal and lymphedema risk. Additionally, intraoperative perfusion assessment reduces anastomotic leak complications in colorectal procedures, while integration with robotic platforms streamlines precision surgical maneuvers across multiple oncologic specialties.
Firefly imaging technology enables surgeons to achieve zero ischemia time during partial nephrectomies by maintaining blood flow to healthy kidney tissue while excising diseased segments. The system provides real-time perfusion data that guides selective vessel clamping, allowing surgeons to target specific vascular structures while preserving circulation to critical areas. This real-time perfusion assessment capability significantly reduces the risk of ischemic damage and enhances surgical precision in complex vascular procedures.
When surgeons achieve zero ischemia time during partial nephrectomy procedures, they eliminate the need for vascular clamping entirely, resulting in superior preservation of renal function compared to traditional cold ischemia techniques. Studies demonstrate minimal postoperative decrease in estimated glomerular filtration rate with zero ischemia approaches, contrasting sharply with the 6.5% decline observed in cold ischemia methods. Firefly imaging enables precise tissue oxygenation monitoring and real-time visualization of renal vasculature, allowing surgeons to perform anatomical vascular microdissection without hilar clamping. This advanced fluorescence guidance facilitates preservation of nephron viability by avoiding ischemic injury entirely. Zero ischemia techniques reduce chronic kidney disease upstaging risks while maintaining oncological safety through negative surgical margins and low complication rates.
Although zero ischemia approaches represent the gold standard for renal preservation, selective vessel clamping offers a strategic middle ground that markedly improves surgical safety through precise vascular management. This technique enables surgical precision enhancement by targeting specific arterial branches while maintaining blood flow to healthy tissue segments. Surgeons achieve superior hemostatic control with reduced overall bleeding compared to total vascular occlusion methods.
Selective clamping facilitates tissue preservation optimization by minimizing ischemic injury to non-targeted areas, resulting in better postoperative organ function and faster recovery. The approach significantly reduces complication rates, particularly acute kidney injury in partial nephrectomy procedures. Enhanced visualization from controlled bleeding supports careful tumor margin delineation while preserving critical vascular structures, ultimately improving both oncologic safety and functional outcomes.
How can surgeons accurately distinguish between viable and compromised tissue during critical procedures when visual assessment alone proves insufficient? Firefly imaging addresses this challenge through real-time perfusion assessment using near-infrared fluorescence with indocyanine green dye. This technology enables precise tissue viability assessment within 30-50 seconds of injection, providing quantitative perfusion data that surpasses subjective visual cues.
During complex surgeries, Firefly imaging supports critical intraoperative decision making by accurately identifying well-perfused versus ischemic tissue segments. Surgeons can immediately adjust resection margins, determine autotransplantation feasibility, or modify surgical approaches based on perfusion quality. This enhanced visualization proves particularly beneficial in procedures like parathyroid preservation during thyroidectomy and ureteral reconstruction, where maintaining tissue importance directly impacts patient outcomes and reduces postoperative complications.
The integration of Firefly imaging technology in surgical procedures significantly reduces postoperative complications through enhanced intraoperative visualization capabilities. Near-infrared fluorescence imaging enables precise identification of anatomical landmarks and vascular structures, minimizing inadvertent tissue injury during surgery. Real-time perfusion assessment using indocyanine green allows surgeons to verify tissue viability before completing anastomoses, substantially reducing anastomotic leak rates.
These improvements directly translate to shortened hospital stays and accelerated patient recovery. Enhanced surgical precision decreases operative trauma while preventing critical postoperative events that typically require extended hospitalization. The technology’s ability to delineate viable tissue margins supports conservative resections, sparing healthy tissue and facilitating faster healing. Decreased reoperation rates result from accurate tumor localization and complete resections, with robotic surgeries utilizing Firefly imaging reporting average recovery periods of approximately six days.
Near-infrared fluorescence technology represents a novel approach in surgical visualization, enabling surgeons to traverse complex anatomical terrain with unparalleled precision. Firefly imaging employs indocyanine green dye that fluoresces under near-infrared light, creating bright real-time contrast for enhanced surgical visualization. This technology integrates seamlessly with robotic platforms, providing surgeons with “night-vision” capabilities that extend beyond standard magnification and lighting. The system enables toggling between normal white light and fluorescence modes for superior intraoperative tissue identification. Magnified 3D fields allow precise identification of critical structures even in fibrotic or scarred tissues. This advanced wayfinding compensates for reduced tactile feedback in minimally invasive procedures, while assisting surgeons in locating structures obscured by previous surgeries or anatomical variations.
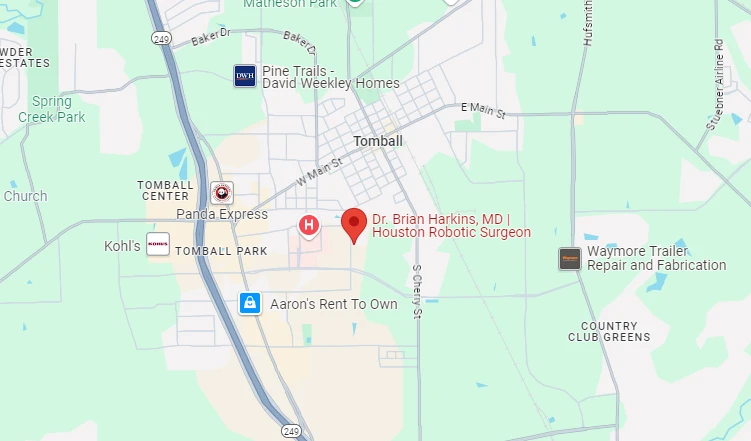
At Dr. Brian Harkins, we are proud to offer Firefly imaging technology as a major advance in surgical precision and patient care. Our Firefly system provides real-time visualization that enables surgeons to distinguish between cancerous and healthy tissue with unparalleled accuracy, while its enhanced blood flow assessment supports optimal intraoperative decision-making. By integrating seamlessly with minimally invasive techniques across multiple specialties, Firefly has helped reduce complications and shorten hospital stays. This fluorescence-guided approach fundamentally improves surgical navigation — delivering greater safety, lower recurrence risk, and superior clinical outcomes for our patients.
While laparoscopic surgery has been the standard for decades, robotic-assisted surgery enhances precision through the da Vinci system. Unlike invasive surgery using standard endoscopic tools, robot-assisted surgery offers greater dexterity, 3D magnification, and integration with advanced imaging systems like firefly fluorescence imaging. Together, these innovations help surgeons perform minimally invasive surgery using smaller incisions while improving outcomes.
Firefly technology offers surgeons real-time visualization of blood flow and tissue viability. By injecting dye and activating near-infrared fluorescent modes, the firefly imaging system is intended to help surgeons see perfusion and vessels invisible under surgery using standard endoscopic visible light. This integration enhances minimally invasive surgical procedures, lowering complications and ensuring safer results.
In rectal cancer patients, precise margin detection is critical. Firefly fluorescence imaging allows surgeons to visualize tumor boundaries and vascular supply intraoperatively. The system enables surgeons to identify risk zones early, reducing risk factors for recurrence. Studies from the National Institutes of Health highlight that fluorescence in robotic procedures improves outcomes in colorectal surgery compared to conventional approaches.
In robotic partial nephrectomy, surgeons rely on indocyanine green fluorescence imaging for real-time assessment of kidney perfusion. This use of indocyanine green highlights vascularized tissue and guides safe resections. The surgeon uses the firefly mode of the da Vinci firefly integration, reducing ischemia time while preserving renal function. Such precision would be far harder with laparoscopic and robotic approaches without this advanced visualization.
Thoracic surgery often involves delicate lymphatic and vascular structures. Intraoperative fluorescence imaging with near-infrared fluorescence imaging with indocyanine provides surgeons with a clear roadmap. When used during robotic surgery, this technology minimizes complications like vessel injury. The firefly imaging system has proven invaluable for pulmonary resections where precision and safety are paramount.
The system is intended for use in identifying tissue perfusion, mapping lymph nodes, and visualizing the common bile duct and common hepatic duct during complex surgeries. The firefly imaging system is intended to be used during robotic surgery with the da Vinci® platform. These indications for use cover multiple specialties, from oncology to reconstructive procedures, providing surgeons superior guidance.
The xi surgical system from Intuitive Surgical seamlessly incorporates fluorescence imaging in robotic-assisted surgery. This means surgeons can toggle between white light and fluorescence imaging of biliary ducts without pausing procedures. Intuitive Surgical develops, manufactures and markets the da Vinci, ensuring intuitive surgical’s mission to advance patient safety with technology continues.
In operations involving biliary ducts with the da Vinci, surgery using firefly provides crucial anatomical differentiation. By enabling fluorescence imaging of biliary ducts, surgeons can clearly see the common bile duct and ducts with the da Vinci, avoiding inadvertent injury. This technology is a new safeguard in minimally invasive surgery using standard approaches where visual clarity is limited.
Not every patient underwent surgery requires Firefly. Surgeons must decide if da Vinci fluorescence is needed depending on procedure type and risk factors. For instance, in urologic surgery and colorectal surgery, use of near-infrared fluorescence imaging is highly beneficial. In other cases, standard visualization may suffice, though surgery may be enhanced by Firefly for safety margins.
Firefly serves as both an enhancement and a safeguard. While it is fully integrated, there are systems intended for standalone use in specific scenarios. Still, as part of the da Vinci surgery suite, firefly technology remains the preferred option to the da Vinci standard workflow. Surgery was performed across multiple specialties, showing how using the da Vinci Firefly consistently improves outcomes.

Dr. Brian Harkins is a renowned surgeon specializing in advanced, minimally invasive, and robotic surgical techniques. With a dedication to innovation and personalized patient care, he has transformed countless lives by delivering exceptional outcomes.
I want a website like this, where do i start?