
Robotic cancer surgery in 2025 refers to the use of advanced robotic surgical systems—such as the Da Vinci Surgical System—to perform precise, minimally invasive cancer operations with outcomes comparable to open and laparoscopic approaches.
Robotic cancer surgery has evolved from a specialized innovation into a global standard across many oncology centers. By 2025, growing evidence demonstrates that robotic resections achieve comparable oncologic margins and long-term survival rates to traditional methods, while offering faster recovery, less blood loss, and shorter hospital stays.
By 2025, robotic surgical systems have transitioned from niche tools to essential components of cancer care. Advances in haptic feedback, miniaturized instruments, and AI-guided imaging have reduced operative time and expanded the scope of minimally invasive resections.
Hospitals increasingly evaluate robotic programs based on:
| Factor | Impact |
| Modular platform design | Lower maintenance and upgrade costs |
| Surgeon experience | Influences learning curve and outcomes |
| Case volume | Drives efficiency and credentialing benchmarks |
| Institutional ROI | Balances patient outcomes and capital investment |
For more on technology adoption in surgery, see recent analyses from the Journal of the American College of Surgeons and NIH PubMed Central.
Recent meta-analyses confirm that robotic resections achieve equivalent or superior negative-margin rates compared to laparoscopic surgery and match open surgery for most solid tumors. Improved 3D visualization and instrument articulation enable greater precision in confined anatomical spaces.
Key margin evaluation practices:
When these practices are standardized, robotic procedures show reduced rates of positive margins and consistent outcomes across institutions.
Survival curves from randomized and registry studies show that when clear margins are achieved, long-term survival and recurrence rates for robotic surgery parallel those of open and laparoscopic cohorts.
Appropriate patient selection remains essential. Multidisciplinary teams weigh tumor characteristics, genetic profiling, and comorbidities when recommending robotic approaches.
| Consideration | Impact on Candidacy |
| Tumor heterogeneity | Determines margin strategy |
| Genetic profile | Guides adjuvant therapy |
| Functional status | Predicts perioperative recovery |
| Clinical trial eligibility | Expands access to emerging indications |
Enhanced optics and tremor-free precision reduce intraoperative blood loss and transfusion needs compared with open surgery. Restrictive transfusion protocols and real-time hemostatic control further enhance safety.
Median hospital stays are typically 1–2 days shorter after robotic cancer surgery. Early mobilization and lower pain scores reduce unplanned readmissions. Standardized discharge education and tele-follow-ups sustain these benefits.
Patients frequently report faster recovery of mobility, continence, and return to work. These benefits are captured using validated patient-reported outcome tools such as EORTC QLQ-C30 and PROMIS scales.
Robotic surgery still carries higher upfront costs due to acquisition and maintenance, but volume-based amortization and reusable instruments are narrowing the gap. Comparative cost-effectiveness depends on fewer complications and shorter hospitalizations.
| Cost Driver | Typical Effect |
| Capital purchase | High upfront |
| Maintenance | Recurring |
| Disposable tools | Per-case expense |
| Case volume | Lowers average cost |
Some payers limit coverage to specific indications. Advocacy for evidence-based reimbursement is ongoing to ensure equitable patient access.
Institutions balance training, scheduling, and equipment use to maximize efficiency and maintain credentialing standards.
Proficiency in robotic oncology depends on structured training and outcome monitoring. Simulation and mentoring shorten learning curves.
| Metric | Benchmark Purpose |
| Case volume | Establish competence |
| Simulation outcomes | Verify skills |
| Complication rates | Track safety |
| Oncologic margins | Confirm quality |
Hospitals now link credential renewal to outcome metrics rather than case numbers alone.
By 2025, robotic cancer surgery achieves oncologic precision and recovery benefits that rival or surpass conventional methods. While survival equivalence is clear, perioperative improvements and patient satisfaction underscore its growing value.
Dr. Brian Harkins and his team remain dedicated to advancing robotic oncology through training, data transparency, and equitable access—ensuring patients benefit from the safest, most effective minimally invasive techniques available today.
Yes, studies show lower blood loss, smaller incisions, and faster recovery, with comparable safety when performed by trained surgeons.
Current evidence indicates similar long-term survival rates to open and laparoscopic approaches when oncologic principles are followed.
Prostate, colorectal, lung, and gynecologic cancers account for the majority of robotic oncologic procedures.
Upfront costs are higher, but shorter hospital stays and fewer complications can offset expenses over time.
Dr. Brian Harkins, among the top 1% of robotic surgeons nationally, integrates advanced Da Vinci techniques and evidence-based protocols to optimize patient outcomes.
Robotic surgery offers greater dexterity, 3D visualization, and wristed instruments, enabling precise dissections that can be challenging with traditional laparoscopy.
While recurrence depends on tumor biology and stage, clear surgical margins achieved with robotic precision can help reduce local recurrence risk.
Most patients experience less pain, smaller scars, and a quicker return to normal activities—often within days to weeks, depending on the procedure.
Yes. Robotic systems require specialized training and may not be suitable for very large or invasive tumors, or for patients with certain health conditions.
Emerging innovations include AI-assisted imaging, haptic feedback, and near-infrared fluorescence guidance, enhancing precision and intraoperative decision-making.
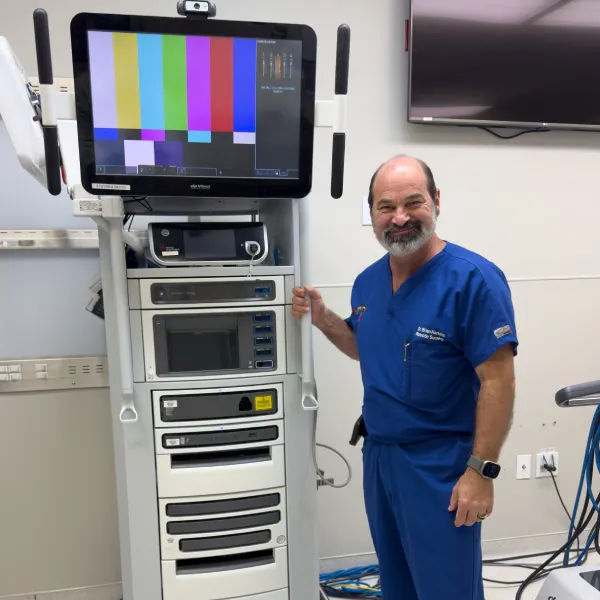


Dr. Brian Harkins is a renowned surgeon specializing in advanced, minimally invasive, and robotic surgical techniques. With a dedication to innovation and personalized patient care, he has transformed countless lives by delivering exceptional outcomes.

I want a website like this, where do i start?