
Intraoperative imaging refers to real-time visualization techniques—such as near-infrared fluorescence, ultrasound, and 3D imaging—used during surgery to enhance precision, assess tissue viability, and guide decision-making.
Modern surgery depends on high-quality intraoperative imaging to visualize anatomy, confirm margins, and guide interventions safely. In 2025, surgeons increasingly rely on near-infrared (NIR) fluorescence, intraoperative ultrasound, and 3D reconstruction to complement one another. Each modality offers unique strengths—NIR for perfusion, ultrasound for depth, and 3D for spatial mapping. Understanding when and how to use each can improve outcomes, reduce complications, and optimize workflow.
When real-time guidance is essential, intraoperative imaging delivers both anatomical and functional data to enhance surgical accuracy. Each modality balances penetration, resolution, and workflow impact:
| Modality | Best For | Limitations |
| NIR Fluorescence | Perfusion & lymphatic mapping | Limited tissue depth |
| Ultrasound (IOUS) | Depth & vessel assessment | Operator-dependent |
| 3D Imaging | Spatial reconstruction | Slower setup, radiation (if CT-based) |
Selecting the right tool depends on the clinical question, required resolution, and workflow impact. For example, NIR may guide vascular perfusion in bowel surgery, while ultrasound may confirm lesion depth during liver resections.
NIR fluorescence relies on light excitation and emission within the near-infrared spectrum. When a fluorophore like indocyanine green (ICG) is injected, specialized cameras detect emitted light, displaying perfusion and lymphatic flow in real time.
| Indication | Use Case |
| Perfusion assessment | Anastomotic integrity in bowel or flap surgery |
| Lymphatic mapping | Sentinel node identification (breast, melanoma) |
| Tumor delineation | Surface margin guidance |
Limitation: NIR only visualizes superficial structures (2–10 mm depth), so it’s best combined with deeper imaging modalities like ultrasound for subsurface confirmation.
Learn more about NIR fluorescence in surgery from NIH Research.
Ultrasound emits high-frequency sound waves that reflect off tissues, creating real-time images of internal anatomy. Doppler modes assess blood flow and vessel patency, while elastography evaluates tissue stiffness for tumor localization.
| Parameter | Importance |
| Probe type | Determines image field and depth |
| Operator skill | Strongly affects accuracy |
| Angle of insonation | Influences Doppler data quality |
Clinical Insight: Intraoperative ultrasound is irreplaceable for lesion localization and margin verification in solid organ and oncologic surgeries. It’s also valuable when optical imaging is limited by blood or gas in the field.
3D imaging provides volumetric reconstructions that reveal complex spatial relationships among organs, tumors, and vessels. It enhances both preoperative planning and intraoperative navigation.
| Scenario | Why 3D Helps |
| Complex reconstructions | Clarifies distorted anatomy |
| Re-operations | Maps scarred or altered landmarks |
| Tumor assessment | Enables volumetric quantification |
| Preoperative planning | Guides incision and trajectory |
Limitation: 3D imaging requires more acquisition time and computational resources, and radiation exposure can be a concern with CT-based systems.
Multimodal imaging often yields the best intraoperative clarity. By combining NIR, ultrasound, and 3D imaging, surgeons can view perfusion, depth, and spatial relationships simultaneously.
| Combined Use | Benefit |
| NIR + Ultrasound | Surface and deep perfusion validation |
| NIR + 3D Imaging | Perfusion overlay on anatomical map |
| Ultrasound + 3D | Depth and spatial correlation for resection planning |
This integration enhances surgical safety, reduces operative uncertainty, and improves confidence during complex procedures.
Adopting multimodal imaging requires careful workflow planning:
| Factor | Impact |
| Capital cost | Affects hospital adoption |
| Maintenance | Influences uptime and performance |
| Technical support | Ensures continuity during surgery |
Selecting the right modality depends on the clinical objective:
| Clinical Goal | Recommended Modality | Key Consideration |
| Vascular perfusion | NIR | Real-time dye kinetics |
| Lesion localization | Ultrasound | Depth and flow evaluation |
| Complex anatomy | 3D Imaging | Spatial reconstruction |
In many cases, surgeons achieve the best outcomes by combining modalities rather than relying on a single imaging method.
At Dr. Brian Harkins, we combine cutting-edge NIR fluorescence, intraoperative ultrasound, and 3D imaging to deliver precision, confidence, and optimal patient care. Each modality serves a specific role, but together they create a more complete surgical picture—enhancing decision-making and safety.
NIR fluorescence is best used for real-time perfusion assessment, flap viability checks, and sentinel lymph node mapping in breast, colorectal, and reconstructive surgeries. It offers instant feedback without radiation exposure.
Intraoperative ultrasound provides depth-resolved, real-time imaging to localize lesions, confirm margins, and evaluate vascular flow. It’s invaluable during liver, kidney, and thyroid procedures where depth visualization is critical.
3D imaging enhances spatial awareness by creating volumetric reconstructions of anatomy. It’s particularly useful in complex reconstructions, tumor resections, and preoperative planning where precision and orientation are essential.
Yes. Combining NIR, ultrasound, and 3D imaging provides a complete picture—surface perfusion, depth structure, and spatial orientation—reducing uncertainty and improving intraoperative decision-making.
Dr. Brian Harkins is among the top 1% of robotic and minimally invasive surgeons nationwide. He routinely integrates multimodal intraoperative imaging to improve safety, accuracy, and patient outcomes.
While NIR offers excellent perfusion and lymphatic visualization, its limited tissue penetration (2–10 mm) restricts its use to surface structures. It should be combined with ultrasound or 3D imaging for deeper tissue visualization.
Like any skill, it requires training and experience, but structured simulation programs and proctored cases help surgeons achieve proficiency quickly. Proper probe selection and image optimization are key to consistent results.
3D imaging provides enhanced depth perception and anatomical clarity, reducing the risk of injury to critical structures. It supports accurate implant positioning, margin assessment, and better intraoperative navigation.
Initially, setup and calibration may add a few minutes, but integrated workflows and trained teams can complete imaging steps rapidly. The accuracy gained often prevents complications and shortens total operative time overall.
Patients should understand that these imaging tools—NIR, ultrasound, and 3D reconstruction—enhance precision and safety. They do not replace the surgeon’s skill but serve as powerful aids in making surgeries safer and more predictable.
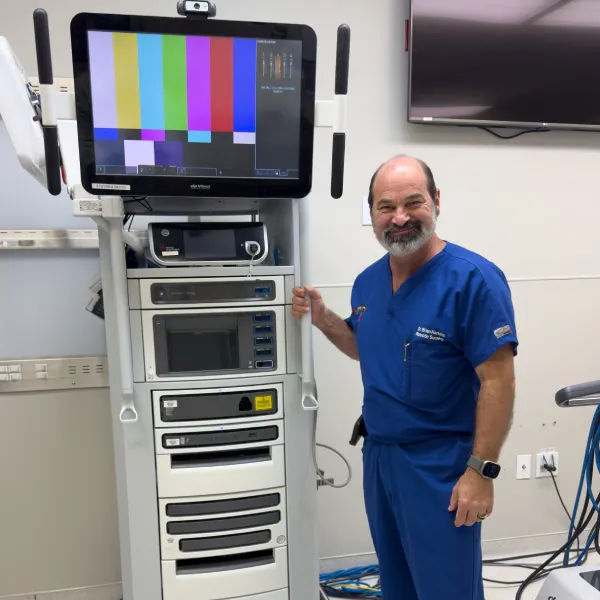


Dr. Brian Harkins is a renowned surgeon specializing in advanced, minimally invasive, and robotic surgical techniques. With a dedication to innovation and personalized patient care, he has transformed countless lives by delivering exceptional outcomes.

I want a website like this, where do i start?