
Enhanced Recovery After Surgery (ERAS) for robotic procedures is a standardized, evidence-based approach that minimizes pain, nausea, and hospital stay by optimizing nutrition, anesthesia, mobility, and recovery protocols.
Enhanced Recovery After Surgery (ERAS) protocols have revolutionized outcomes in robotic and minimally invasive surgery. By focusing on every step—from preoperative nutrition and medication management to postoperative mobilization and discharge—ERAS protocols promote faster recovery, reduced complications, and improved patient satisfaction.
These checklists replace traditional, fragmented care with coordinated, multidisciplinary plans designed for consistency and safety. Let’s explore how each phase contributes to a smoother, pain-free recovery after robotic surgery.
Proper preparation begins well before surgery. A focused preoperative plan addresses nutrition, medications, and patient engagement:
These measures build patient confidence, reduce anxiety, and improve adherence to postoperative recovery milestones.
Traditional fasting causes catabolism and dehydration. ERAS guidelines allow:
Patients typically receive a 12.5–50g carbohydrate drink the evening before and another 2–3 hours preoperatively. This reduces insulin resistance, promotes comfort, and improves hemodynamic stability.
For detailed ERAS nutrition standards, visit ERAS Society Guidelines.
ERAS encourages a multimodal approach to pain:
Opioids are reserved for breakthrough pain, minimizing side effects and improving early mobility. Consistent dosing, documentation, and tapering protocols ensure safe recovery.
Postoperative nausea and vomiting (PONV) delays recovery and causes discomfort. ERAS protocols use risk-stratified, multimodal prevention:
Non-drug measures—hydration and limiting volatile anesthetics—enhance results.
This structured approach lowers unplanned admissions and improves patient experience.
Robotic procedures already offer improved dexterity and visualization. ERAS builds on this by promoting:
This minimizes inflammation, bleeding, and postoperative pain.
ERAS emphasizes goal-directed fluid therapy:
Stable hemodynamics preserve organ perfusion during pneumoperitoneum and patient positioning—critical during robotic operations.
Early movement enhances recovery, reduces pulmonary complications, and shortens hospital stays.
Patients are encouraged to:
Use pedometers or hospital monitors to track progress and motivate activity. Reaching daily goals correlates with fewer complications and quicker bowel recovery.
Physical therapy adds progressive resistance and mobility tasks—sit-to-stand exercises, stair climbing, and balance training—monitored through measurable milestones.
Patients can often start clear liquids within hours post-op, advancing to soft foods as tolerated. Early intake reduces ileus, supports healing, and improves satisfaction.
Combining medications like 5-HT3 antagonists, dexamethasone, and dopamine blockers ensures tolerance and limits nausea:
| Drug Class | Mechanism | Practical Use |
| 5-HT3 antagonists | Serotonin blockade | First-line for most patients |
| Dexamethasone | Anti-inflammatory | Single-dose benefit |
| NK-1 antagonists | Substance P blockade | For high-risk cases |
| Dopamine antagonists | D2 blockade | Rescue therapy |
Patients are discharged only after meeting standardized milestones:
Before discharge, caregivers receive clear instructions on red-flag symptoms and contact numbers. Post-discharge support includes follow-up calls, wound checks, and outpatient rehabilitation plans to reduce readmissions.
At Dr. Brian Harkins, we combine ERAS principles with advanced robotic surgical technology to deliver safer, faster recoveries. By standardizing care—from nutrition and pain control to early mobility and discharge—we minimize complications and enhance comfort.
ERAS aims to enhance patient recovery by reducing pain, nausea, and length of hospital stay through standardized, evidence-based care steps.
Yes. ERAS can be adapted for most general, colorectal, urologic, and gynecologic robotic surgeries, with specialty-specific adjustments.
It prevents muscle breakdown, reduces insulin resistance, and stabilizes metabolism—helping patients feel stronger and recover faster.
Not entirely. They’re used as rescue medication when necessary but minimized in favor of non-opioid pain strategies.
Most patients start clear fluids within hours post-op, advancing to solid food as tolerated, promoting faster bowel recovery.
Moving soon after surgery prevents pneumonia, blood clots, and muscle loss—leading to faster recovery and shorter stays.
ERAS replaces reactive care with proactive, standardized protocols, reducing variability and focusing on rapid, safe recovery.
A multidisciplinary team—including surgeons, anesthesiologists, nurses, and physical therapists—coordinates ERAS pathways for each patient.
Yes, when tailored. Adjustments are made for comorbidities, ensuring safety while still promoting faster, evidence-based recovery.
Dr. Brian Harkins integrates robotic precision with ERAS best practices, ensuring minimal pain, low complication rates, and shorter hospital stays for his patients.
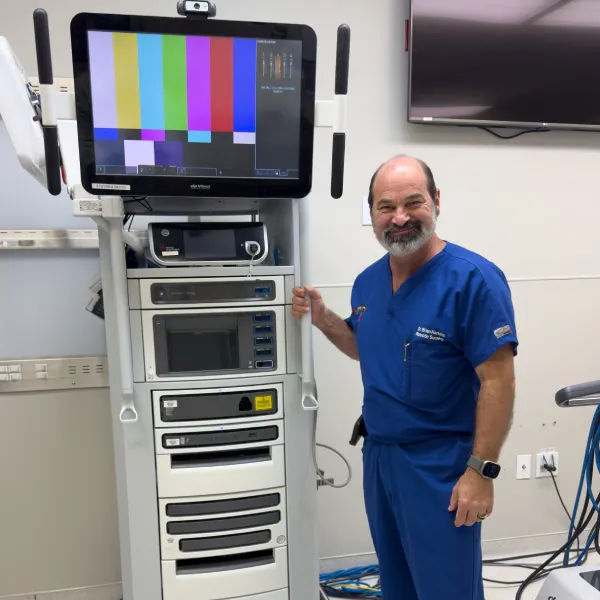


Dr. Brian Harkins is a renowned surgeon specializing in advanced, minimally invasive, and robotic surgical techniques. With a dedication to innovation and personalized patient care, he has transformed countless lives by delivering exceptional outcomes.

I want a website like this, where do i start?