
Combining low-pressure insufflation, Enhanced Recovery After Surgery (ERAS) protocols, AI-driven perioperative management, and multimodal pain relief creates a powerful, evidence-based strategy to reduce pain, complications, and recovery time in minimally invasive surgery.
Modern robotic and laparoscopic surgery continues to evolve toward precision, personalization, and faster recovery. By integrating low-pressure CO₂ insufflation, Enhanced Recovery After Surgery (ERAS) protocols, AI-guided perioperative optimization, and multimodal analgesia, surgical teams can significantly reduce pain, complications, and hospital stays while improving patient comfort and safety.
This holistic, data-driven approach reflects the next generation of minimally invasive care—one where technology, teamwork, and patient-centered design come together for optimal outcomes.
Standard pneumoperitoneum pressures can strain the heart, lungs, and abdominal organs. Lowering insufflation to 7–10 mmHg reduces:
Low-pressure techniques are particularly beneficial for:
These physiologic advantages translate into fewer respiratory complications and faster recovery without compromising visualization.
See SAGES Guidelines for recommendations on optimal pneumoperitoneum management.
ERAS is an evidence-based framework designed to standardize perioperative care and promote early return to function.
Key ERAS Elements Include:
| ERAS Component | Purpose |
| Preoperative counseling | Reduces anxiety, aligns expectations |
| Carbohydrate loading | Prevents catabolism, stabilizes glucose |
| Opioid-sparing analgesia | Reduces side effects, promotes mobility |
| Goal-directed fluid therapy | Prevents overload, supports perfusion |
| Early mobilization | Shortens hospital stay, prevents complications |
When implemented with minimally invasive surgery and low-pressure insufflation, ERAS protocols enhance consistency, safety, and outcomes.
Artificial intelligence (AI) is revolutionizing perioperative care by analyzing real-time data to optimize fluid and ventilation management.
AI-Guided Adjustments Include:
AI decision-support systems act as an intelligent “co-pilot,” alerting clinicians to deviations and suggesting evidence-based interventions. This reduces variability and enhances safety across complex procedures.
Multimodal analgesia targets multiple pain pathways using both pharmacologic and nonpharmacologic methods:
Each approach contributes to the same goal—reducing surgical stress and optimizing recovery—but their combined effects are synergistic, not merely additive.
| Approach | Primary Benefit | Synergistic Effect |
| Low-pressure insufflation | Reduces cardiopulmonary stress | Enhances physiologic tolerance |
| ERAS protocol | Standardizes recovery pathway | Improves consistency and efficiency |
| AI management | Personalizes fluid and ventilation | Enables real-time optimization |
| Multimodal pain relief | Lowers opioid use | Reduces systemic side effects |
This integrated model aligns perfectly with modern robotic and laparoscopic workflows, creating a personalized, data-driven recovery experience.
By addressing these barriers proactively, institutions achieve smoother rollouts and higher protocol adherence.
Ongoing monitoring is key to refining ERAS and low-pressure practices.
Essential Metrics Include:
Dashboards and automated data collection systems ensure real-time insights that support continuous quality improvement and accountability.
Innovation continues to push boundaries in surgical recovery:
| Innovation | Impact |
| Robotic assistance | Enhances precision and reduces trauma |
| Telemedicine integration | Supports pre- and post-op follow-up |
| AI analytics | Predicts outcomes and refines recovery timing |
| Surgical simulation | Improves team readiness and efficiency |
These technologies will make personalized, AI-driven, and low-stress surgical care the new standard.
At Dr. Brian Harkins, we bring together the best in surgical science and technology—low-pressure insufflation, ERAS protocols, AI-guided management, and multimodal pain control—to deliver safer, faster, and more personalized recovery experiences.
Through precision techniques and multidisciplinary teamwork, we continue to refine minimally invasive care for optimal outcomes and long-term health.
It’s a laparoscopic technique using 7–10 mmHg of CO₂ pressure—lower than standard—to minimize cardiopulmonary stress and postoperative pain.
ERAS reduces variability in care by standardizing perioperative steps, promoting early mobilization, and minimizing opioid dependence for faster recovery.
Yes. AI systems analyze real-time data to optimize fluid balance, ventilation, and blood pressure, helping surgeons and anesthesiologists maintain stability.
It targets multiple pain pathways, allowing reduced opioid use while maintaining strong, consistent pain relief.
Yes, when personalized. High-risk or elderly patients often benefit the most from low-pressure insufflation and AI-driven stability monitoring.
Implementation requires coordination, but once standardized, the workflow becomes more efficient and outcomes are significantly better.
Dr. Harkins leads in implementing AI-assisted, ERAS-guided robotic surgery, ensuring each patient benefits from the safest and most advanced care methods available.
Studies show that low-pressure CO₂ insufflation significantly reduces shoulder tip and incision pain after laparoscopic or robotic surgery. This translates to lower opioid requirements and improved patient comfort during recovery.
Procedures such as hernia repairs, cholecystectomies, colorectal surgeries, and gynecologic operations benefit greatly from combining low-pressure insufflation, ERAS, and AI-guided techniques due to reduced inflammation, faster healing, and shorter hospital stays.
Most patients resume light activities within a few days and return to normal function within one to two weeks, depending on the procedure type and individual health factors. Early mobility and optimized pain control under ERAS protocols accelerate recovery safely.
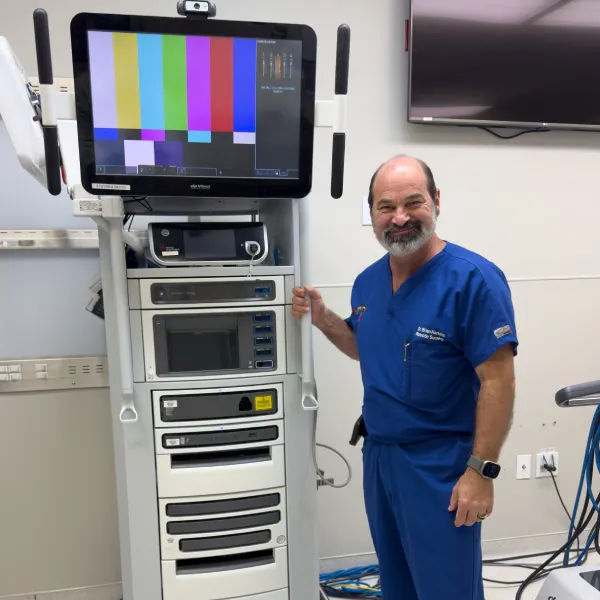


Dr. Brian Harkins is a renowned surgeon specializing in advanced, minimally invasive, and robotic surgical techniques. With a dedication to innovation and personalized patient care, he has transformed countless lives by delivering exceptional outcomes.

I want a website like this, where do i start?