
Low-pressure CO₂ insufflation is a minimally invasive surgical technique using 7–10 mmHg abdominal pressure—lower than standard levels—to reduce pain, cardiopulmonary strain, and recovery time while maintaining safe visualization during robotic or laparoscopic surgery.
Low-pressure insufflation has become an important refinement in laparoscopic and robotic surgery, especially for patients who benefit from reduced intra-abdominal pressure and improved comfort. By limiting pressure to 7–10 mmHg instead of the standard 12–15 mmHg, this approach minimizes cardiopulmonary stress, postoperative pain, and nausea—particularly in elderly patients or those with cardiopulmonary conditions.
While visualization can be slightly more challenging at lower pressures, advancements in imaging, smoke evacuation, and CO₂ regulation have made this method safe and reproducible across many surgical specialties.
Low-pressure CO₂ insufflation minimizes the hemodynamic and respiratory changes caused by standard pneumoperitoneum. By lowering intra-abdominal pressure, surgeons preserve venous return, cardiac output, and pulmonary compliance while reducing diaphragm displacement.
Patients who may benefit most include:
Low-pressure may not be suitable for:
Selection balances the need for exposure against patient physiology to ensure safety and efficiency.
| Parameter | Target Range | Purpose |
| Pressure | 7–10 mmHg (low-pressure) | Reduces cardiopulmonary strain |
| Temporary increase | 12–15 mmHg | Improves visualization if needed |
| Flow rate (initial) | 4–6 L/min | Achieves target pressure quickly |
| Flow rate (maintenance) | 1–3 L/min | Minimizes peritoneal stretch and discomfort |
Pro Tip: Use incremental insufflation and real-time monitoring to stabilize pressure during instrument exchange or suctioning.
Reduced abdominal distension can make visualization challenging. Surgeons can enhance exposure with the following techniques:
These techniques preserve exposure quality while maintaining the physiologic advantages of low-pressure insufflation.
Learn more about intra-abdominal pressure management from SAGES guidelines.
Multiple randomized controlled trials have demonstrated the safety and comfort benefits of low-pressure CO₂ insufflation compared with standard pressure techniques.
| Outcome | Low-Pressure Advantage | Evidence Summary |
| Shoulder & incision pain | Reduced | Less diaphragmatic irritation and CO₂ absorption |
| Recovery time | Shorter | Early ambulation and discharge |
| Opioid use | Lower | Improved multimodal analgesia integration |
| Complications | Similar | No significant difference in major adverse events |
Patients report better short-term comfort without compromising procedural outcomes when low-pressure protocols are properly implemented.
Low-pressure insufflation excels in specific cases:
For complex oncologic, bariatric, or multi-quadrant surgeries, visualization demands may outweigh the physiologic gains. In such cases, hybrid strategies using intermittent pressure increases can strike an ideal balance.
At Dr. Brian Harkins, we advocate for low-pressure CO₂ insufflation when patient physiology and surgical goals align. This method offers a safe, evidence-based way to reduce pain, cardiopulmonary strain, and recovery time—especially in high-risk or elderly patients.
By tailoring pressure settings, employing visualization adjuncts, and closely monitoring intraoperative conditions, our team ensures that each patient benefits from precision, safety, and comfort throughout their robotic or laparoscopic procedure.
It’s a minimally invasive technique that uses reduced CO₂ pressure (7–10 mmHg) to create pneumoperitoneum, decreasing strain on the heart and lungs compared with standard 12–15 mmHg levels.
Elderly patients and those with heart, lung, or obesity-related conditions benefit from reduced cardiopulmonary stress and faster recovery.
It can, but using angled scopes, smoke evacuation, and humidified CO₂ helps maintain optimal visualization. Temporary pressure increases are also possible when needed.
No. It’s ideal for short or less complex procedures, but not always suitable for large oncologic or bariatric cases requiring wide exposure.
Yes. Studies show reduced shoulder tip and incision pain, which often translates to lower opioid use and quicker mobility.
Anesthesiologists appreciate low-pressure approaches because they maintain better respiratory compliance and lower airway pressures during surgery.
Yes. Pressures below 6 mmHg can compromise visualization and increase operative time. Maintaining balance is key.
Smart insufflation systems use feedback control to maintain steady flow rates (1–3 L/min) and prevent pressure spikes during instrument exchanges.
Patients undergoing low-pressure insufflation often experience faster recovery and earlier discharge, thanks to reduced shoulder pain, less inflammation, and fewer cardiopulmonary effects. Most can resume normal activities sooner compared with standard-pressure cases.
Absolutely. Low-pressure insufflation integrates seamlessly with robotic platforms like the Da Vinci Surgical System, offering enhanced control, visualization, and ergonomics while maintaining patient safety and comfort.
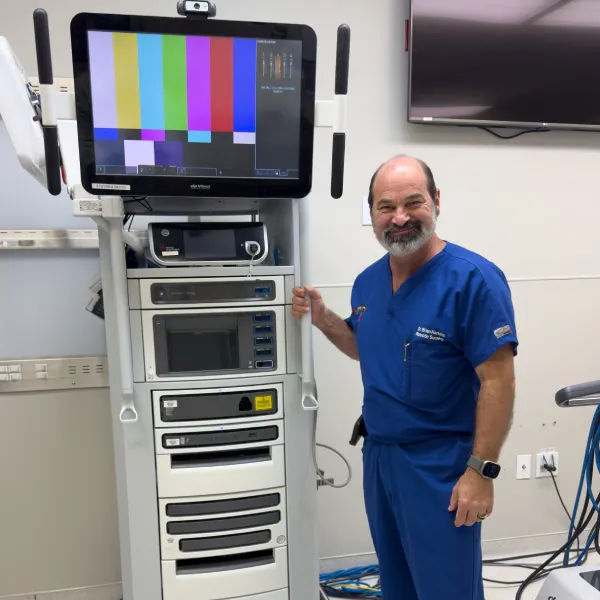


Dr. Brian Harkins is a renowned surgeon specializing in advanced, minimally invasive, and robotic surgical techniques. With a dedication to innovation and personalized patient care, he has transformed countless lives by delivering exceptional outcomes.

I want a website like this, where do i start?