Recent breakthroughs in minimally invasive surgery include the revolutionary Da Vinci 5 System with 10,000x greater computing power and force feedback technology. Miniaturized robotics now achieve 0.2mm positioning precision, while AI-optimized implant positioning reaches mean deviations of just 1mm from planned positions. Robotic spine surgery demonstrates 99.6% accuracy in pedicle screw placement with sub-millimeter precision. Machine learning enhances real-time surgical decision making through predictive analytics achieving AUROC scores up to 0.972. These innovations promise even greater surgical alterations ahead.
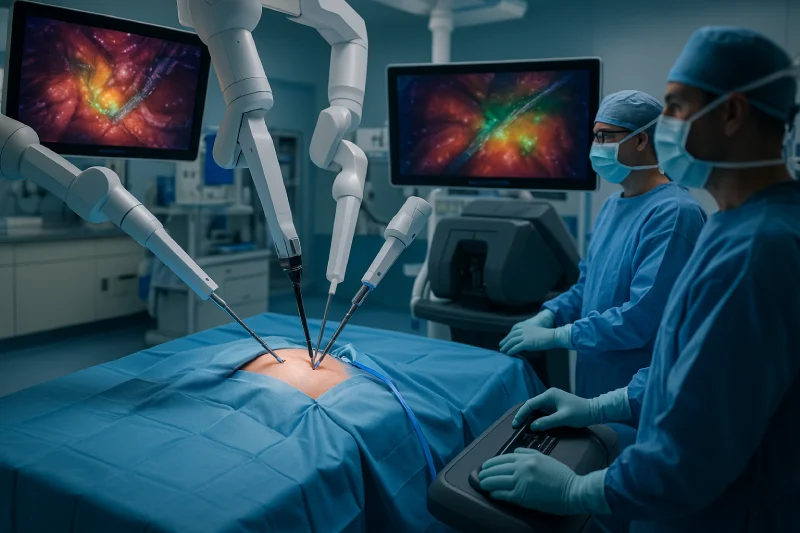
The Da Vinci 5 system represents a quantum leap in robotic surgical technology, integrating over 150 design innovations with computing power that exceeds previous models by a factor of 10,000. This advancement enables revolutionary force feedback technology, allowing surgeons to sense tissue tension remotely—a capability that reduces applied force by up to 40% and minimizes tissue trauma. The system’s enhanced artificial intelligence facilitates expert opinion integration through real-time collaboration tools and objective performance analytics. Superior high-definition 3D visualization provides crystal-clear surgical field views, while improved console ergonomics reduce surgeon fatigue. The My Intuitive+ digital platform supports procedure customization through personalized training and performance data analysis, enabling AI-powered task automation that streamlines workflow and reduces operating room time significantly. This technology enables procedures across multiple specialties including cardiac, urologic, gynecologic, pediatric, and general surgery.
While larger robotic systems have dominated surgical suites for decades, miniaturized robotics now represents the next evolutionary step in minimally invasive surgery, providing unparalleled precision while dramatically reducing patient trauma and recovery times. These compact systems achieve singular accuracy, with devices like the Intelligent SpinePecker achieving 0.2mm positioning precision for pedicle screw placement. Enhanced operator control through integrated computer vision and haptic feedback enables surgeons to traverse confined surgical fields with unmatched dexterity. Studies demonstrate significant benefits, including zero conversions to open surgery and median hospital stays reduced to two days. Optimized implant fixation through handheld micro-robotic platforms like THINK Surgical’s TMINI Robot certifies accurate placement while maintaining workflow integration, ultimately expanding robotic surgery accessibility across specialties. The integration of artificial intelligence in these miniaturized systems further enhances surgical precision by providing real-time analysis and decision support during procedures.
Artificial intelligence has revolutionized implant surgery by providing exceptional positioning accuracy, with AI-driven robotic systems like X-Guide flexible guidance and Yomi robotic assist achieving mean deviations of just 1mm from pre-planned implant positions compared to significantly greater variances in traditional freehand methods. These systems analyze patient-specific medical history, bone density, and anatomical data to generate customized treatment plans that optimize implant dimensions and placement. Real-time AI direction enables continuous feedback during surgery, facilitating intraoperative complication avoidance by helping surgeons adjust interventions to prevent damage to critical structures like nerves and blood vessels. Patient specific implant design through AI recommendations improves integration outcomes while reducing surgical trauma, shortening recovery times, and minimizing revision surgery needs through enhanced precision. AI algorithms analyze X-rays and CT scans with remarkable accuracy to identify optimal implant placement locations and assess bone quality for anticipating potential complications.
Machine learning algorithms now enable surgeons to optimize implant positioning through AI-driven analysis of patient anatomy and biomechanical modeling during minimally invasive procedures. Real-time anatomical recognition systems process surgical video streams to identify critical structures and delineate safe zones, providing immediate visual guidance to surgical teams. These predictive systems analyze intraoperative data to forecast potential complications and surgical outcomes, allowing surgeons to make informed adjustments throughout the procedure. Advanced automated machine learning approaches tackle the challenge of highly imbalanced surgical action datasets to enable rapid deployment of real-time surgical training systems.
How can surgeons achieve unparalleled precision in implant placement while simultaneously reducing operative time and complications? AI-optimized implant positioning systems now deliver real-time guidance that alters surgical precision. Machine learning algorithms analyze patient-specific data including bone density, anatomical features, and medical history to determine optimal implant size, angle, and position with unmatched accuracy.
Commercial systems like Stryker’s MAKO™ provide automated templating and intraoperative support, while AI tools achieve up to 99% accuracy in implant identification from radiographic images. These systems enable implant failure prediction by identifying high-risk factors and support implant selection optimization through rapid analysis of multidimensional datasets. Runtime speeds of just eight seconds per radiograph allow seamless workflow integration, while AI delineates anatomical landmarks with 100% accuracy in specific settings, substantially reducing human error during critical positioning decisions.
What happens when surgeons can instantly identify critical anatomical structures and surgical phases with unparalleled accuracy during live operations? AI-driven real-time recognition systems are revolutionizing surgical precision through sophisticated CNN-LSTM models that achieve over 91% accuracy in laparoscopic procedures. These systems operate at 32 frames per second, providing seamless intraoperative feedback while automated tissue segmentation identifies critical structures like nerves and blood vessels during colorectal surgery.
Augmented reality overlays enhance anatomical visualization, particularly benefiting neurosurgical procedures by delineating critical boundaries during tumor resection. AI-assisted pathological lesion detection significantly outperforms novice surgeons in tumor staging accuracy, reducing risks of inappropriate treatment plans. This unified surgical intelligence integrates spatial feature extraction with temporal transition analysis, creating inclusive decision support systems that enhance both surgical education and patient safety through real-time anatomical guidance.
Revolutionary advances in machine learning are altering surgical decision-making through predictive models that achieve exceptional accuracy rates, with some automated systems reaching AUROC scores of 0.972 for mortality prediction using only preoperative variables. These sophisticated algorithms consistently outperform traditional risk calculators by approximately 0.048 AUROC, demonstrating superior predictive modeling accuracy across various surgical complications.
Preoperative risk stratification has been augmented through machine learning’s ability to analyze multisource data including demographics, clinical variables, and situational factors. Key predictors such as anemia levels, blood transfusion requirements, and patient location enable personalized risk profiles previously unavailable. Gradient enhanced models achieve AUCs of 79-87% while maintaining excellent calibration scores.
This enhanced predictive capability enables targeted perioperative interventions, optimized resource allocation, and improved patient selection, ultimately reducing complications and mortality rates.
While traditional spine surgery has long relied on surgeon experience and basic imaging guidance, robotic-assisted systems are now providing unparalleled precision in critical procedures like pedicle screw placement. Studies demonstrate that robotic platforms achieve up to 99.6% accuracy rates, significantly outperforming both localization and freehand techniques with odds ratios of 2.02 and 3.06 respectively.
| Technology Feature | Benefit |
| Sub-millimeter precision | Optimal screw trajectories |
| Reduced fluoroscopy | Lower radiation exposure |
| Real-time confirmation | Immediate corrections |
| Haptic feedback integration | Enhanced surgeon control |
| Telerobotics applications | Remote surgical capabilities |
These systems eliminate hand tremor while providing enhanced visualization and planning tools. Machine learning integration enables predictive analytics for personalized surgical planning, while encoder-based tracking surpasses optical methods in precision.
As surgical precision reaches new heights through robotic assistance, augmented reality technology is altering operating rooms into hybrid environments where digital overlays seamlessly merge with physical anatomy. AR systems integrate real-time patient data without replacing conventional monitors, creating an additional information layer that enhances surgical workflows. Stanford and other leading institutions demonstrate how surgeons can quickly review and manipulate intraoperative data through intuitive AR interfaces, reducing cognitive load while improving clinician satisfaction.
These hybrid environments enable holographic surgical guidance, allowing surgeons to visualize 3D anatomical structures with millimeter accuracy. The technology facilitates remote surgical collaboration, connecting specialists across distances for complex procedures. Future applications include enhanced surgical education and augmented procedural direction through spatial computing, promising significant improvements in patient outcomes and surgical efficiency.
High-definition visualization technology has emerged as a critical factor in reducing surgeon fatigue during minimally invasive procedures, with studies demonstrating that enhanced image clarity significantly decreases eye strain and cognitive load throughout extended operations. Advanced HD systems enable surgeons to operate for longer periods while maintaining precision and focus.
| Traditional Visualization | HD Visualization |
| Frequent eye strain | Reduced fatigue levels |
| Limited depth perception | Enhanced 3D imaging |
| Poor ergonomic positioning | Improved ergonomics |
| Higher complication rates | Better safety outcomes |
| Shorter operative tolerance | Extended procedure capability |
The technology’s impact extends beyond comfort, directly improving patient safety through clearer identification of anatomical structures. Enhanced visualization combined with improved ergonomics creates optimal surgical conditions, reducing risks while enabling more precise interventions in complex procedures.
How can surgeons achieve unparalleled precision in joint replacement procedures? AI-guided arthroplasty systems are revolutionizing surgical outcomes by dramatically reducing malposition rates through customizable ai guidance technology. These systems increase acetabular component size prediction accuracy to 84.1% compared to 64.0% with conventional planning, while achieving conformity rates of 90.9% for acetabular cups and 87.3% for femoral stems.
The technology guarantees implant placement within recommended safe zones, significantly reducing dislocation risks and limb length discrepancies. Retrospective studies demonstrate lower malposition rates and fewer postoperative complications when utilizing AI-based preoperative planning. Optimized femoral stem alignment contributes to enhanced implant longevity by reducing loosening and failure risks. Additionally, AI automation reduces surgeon corrections by 39.7% while standardizing templating protocols, creating more reproducible outcomes across varied patient anatomies.
False assumptions about minimally invasive surgery’s limitations are being shattered as cross-specialty applications demonstrate extraordinary expansion capabilities. Neurosurgeons now achieve enhanced tumor localization and precise pedicle screw placement, while general surgeons employ robotic-assisted techniques for improved gastrointestinal outcomes. Gynecologic specialists increasingly adopt Single-Incision Laparoscopic Surgery and Natural Orifice Transluminal Endoscopic Surgery, offering patients reduced pain and faster recovery times.
The global market’s projected growth to $73.4 billion by 2025 reflects this cross-pollination of techniques. AI-enhanced tools and robotic systems provide surgeons with superior visualization and control across specialties. However, reduced medicolegal risks emerge as standardized protocols develop, while ethical considerations in innovation require careful balancing of technological advancement with patient safety standards and surgeon training requirements.
Within two decades, day surgery has fundamentally altered perioperative care, now accounting for 60-70% of elective procedures in developed countries. The 23-hour surgery model demonstrates exceptional success rates, with most patients achieving functional recovery within two weeks while maintaining low readmission rates of just 2%.
| Recovery Metric | Timeline | Success Rate |
| Functional Recovery | 14 days | 85-90% |
| Patient Readmission | 30 days | 2% |
| Provider Contact | Post-discharge | 25% |
This shift emphasizes personalized pain management strategies that address individual recovery trajectories rather than static protocols. Digital care pathways now provide 24/7 guidance through online instructions and symptom navigators, enhancing patient self-management capabilities. Enhanced Recovery After Surgery protocols support accelerated discharge without compromising safety, revamping traditional inpatient experiences into streamlined outpatient procedures.
At Dr. Brian Harkins, we view these technological advances as reshaping the landscape of surgical practice and fundamentally elevating patient care standards. Our integration of robotics, artificial intelligence, and enhanced visualization systems establishes new benchmarks for precision, safety, and recovery outcomes. As we continue to expand and refine these innovations across medical specialties, we are committed to making complex procedures more accessible while consistently reducing patient trauma and healthcare costs through improved efficiency and shortened hospital stays.
Laparoscopy introduced the foundation for minimally invasive techniques, enabling surgeons to perform complex abdominal surgery through a small incision instead of large cuts. This less invasive approach has significantly reduced trauma, resulting in less pain, shorter hospital stays, and improved clinical outcomes across a variety of medical specialties.
Recent advances and new advancements include the da Vinci surgical system, which combines robotic arms with high-definition visualization. These advancements in minimally invasive surgery enable greater precision in robotic approaches like robot-assisted surgery, bariatrics, and gynecologic surgery, delivering safer and more efficient surgical techniques.
Unlike traditional surgery, which relies on large open surgical incisions, minimally invasive surgical procedures use minimal access and advanced surgical instruments. This surgical approach provides less invasive procedures, faster healing, and lower recurrence rates, while allowing surgeons to perform surgery with enhanced accuracy.
Robotic procedures, particularly those using robotic technology and using robotic systems, deliver unprecedented precision in surgical management. These robot-assisted interventions enhance dexterity and control, improving clinical outcomes across specialties such as pediatric surgery, colorectal cancer, and invasive surgical procedures.
A laparoscopic approach relies on rigid instruments and 2D views, while robotic vs laparoscopic surgery highlights the advantages of robotic technology, including 3D visualization and tremor filtration. Both laparoscopic and robotic approaches are less invasive surgical techniques, but robotics often achieves superior precision.
Minimally invasive coronary artery bypass and coronary artery bypass grafting represent major breakthroughs in invasive cardiac surgery. Unlike traditional open-heart surgery, these minimally invasive coronary approaches use smaller incisions, reduce trauma, and achieve comparable clinical outcomes, making them standard in many surgery programs.
For hernia repair and bariatric surgery, advances in minimally invasive surgery deliver less invasive procedures with lower complication risks. Techniques such as laparoscopic cholecystectomy, video-assisted thoracoscopic surgery, and robotic approaches provide durable solutions with reduced recurrence rates.
In gynecologic surgery, robot-assisted surgery provides precise robotic arms that enhance surgical techniques. These robotic approaches are particularly beneficial for complex pelvic conditions. Clinical trial results show improved surgical management and better surgical outcomes when advanced technology is used in including minimally invasive interventions.
Laparoscopic and robotic approaches have transformed gastrointestinal surgery and other abdominal interventions. These minimally invasive surgical techniques minimize tissue trauma, accelerate recovery, and improve outcomes in procedures like colorectal cancer resections, surpassing the risks associated with versus open techniques.
The future of minimally invasive surgical practice emphasizes new minimally invasive tools such as AI-powered imaging, robotic arms, and augmented visualization. With data from consecutive cases, surgeons continue refining surgery in modern practice, demonstrating that advancements in minimally invasive surgery consistently improve surgical safety and efficiency.

Dr. Brian Harkins is a renowned surgeon specializing in advanced, minimally invasive, and robotic surgical techniques. With a dedication to innovation and personalized patient care, he has transformed countless lives by delivering exceptional outcomes.

I want a website like this, where do i start?