
Robotic surgery offers numerous benefits for cancer care. It enhances precision and accuracy in tumor removal, leading to improved patient outcomes and survival rates. The minimally invasive approach reduces scarring and shortens recovery times. Additionally, robotic surgery results in lower complication rates and improved postoperative experiences. By automating tasks and providing real-time feedback, robotic systems optimize procedures. With advancements in technology on the horizon, there are even more benefits to investigate in robotic cancer surgery.
Robotic surgery has significantly evolved as a revolutionary approach in cancer treatment, integrating advanced technology to enhance surgical precision. This innovative technique is reshaping the environment of oncology by offering key benefits such as improved visualization and reduced recovery times. As robotic-assisted surgery becomes more prevalent, understanding its features and impact on patient outcomes is essential for both practitioners and patients alike. Studies indicate that robotic surgeries have a higher success rate than laparoscopic surgeries for cancer treatment, further establishing its effectiveness in clinical practice.
As advancements in technology reshaped the terrain of medicine, the field of cancer surgery began to adopt innovative approaches that enhanced surgical precision and minimized patient trauma. The evolution of robotic surgery has marked a significant shift in surgical oncology, highlighting the benefits of robotic surgery for cancer care. Key developments include:
This alteration emphasizes the advantages of robotic surgery vs traditional surgery for cancer, showcasing how advancements in robotic surgery technology have led to improved patient outcomes and quicker recovery times. Furthermore, the use of sophisticated systems has transformed the landscape of surgical procedures, allowing for greater flexibility and access to challenging anatomical areas.
Changing the terrain of cancer treatment, robotic surgery is revolutionizing how surgical procedures are performed. This innovative approach offers numerous robotic-assisted cancer surgery advantages, including enhanced precision and reduced complications. By utilizing smaller incisions, robotic-assisted surgery minimizes trauma to surrounding tissues, resulting in less blood loss and a lower risk of infection. These factors contribute to improved patient outcomes with robotic oncology procedures, allowing for faster recovery with robotic-assisted surgery. Patients often experience shorter hospital stays and can quickly resume normal activities, accelerating the initiation of additional treatments like chemotherapy. As robotic technology advances, its role in cancer care continues to expand, offering hope for more effective and less invasive treatment options. Furthermore, the commitment to minimally invasive surgical techniques has been a cornerstone of UI Health’s approach to enhancing patient care in robotic surgery.
The scenery of surgical oncology has been significantly enhanced by the introduction of robotic-assisted surgery. This innovative approach offers several key features that improve patient care and surgical outcomes:
Robotic surgery greatly improves the precision and accuracy of tumor removal. With advanced real-time 3D imaging and robotic arms that mimic the surgeon’s movements, the technology allows for careful control and dexterity, minimizing damage to surrounding healthy tissue. This approach not only improves visualization but also guarantees that tumor resections are targeted and effective.
Surgical precision has evolved significantly with the integration of advanced robotic systems in cancer care. These systems enhance surgeon control and dexterity, leading to numerous robotic tumor removal benefits. Key factors include:
These advancements in precision oncology with robotic surgery yield targeted approaches for tumor removal, minimizing damage to healthy tissues and improving patient outcomes.
Advancements in surgical technology have led to the integration of real-time 3D imaging, significantly enhancing tumor visualization during procedures. This innovative approach allows for precise tumor localization by generating detailed three-dimensional models of patient anatomy. When combined with robotic-assisted techniques, the benefits are significant, as surgeons gain real-time observations that facilitate accurate tumor resection. The fusion of preoperative 3D images with intraoperative data further enhances decision-making and guidance through complex structures. AI in robotic-assisted cancer surgery plays a crucial role, improving surgical accuracy and outcomes. Overall, these advancements in imaging technology contribute to the effective removal of tumors while minimizing damage to surrounding healthy tissues, ultimately advancing the field of robotic prostate cancer surgery.
Precision in tumor removal has become a hallmark of modern cancer treatment, significantly reducing damage to surrounding healthy tissue. Robotic lung cancer surgery advancements and robotic colorectal cancer surgery success rates demonstrate the effectiveness of these techniques.
Key benefits include:
As the future of robotic-assisted surgery in oncology unfolds, the enhanced precision and accuracy of robotic systems continue to improve surgical margins, leading to better preservation of healthy tissue and overall patient well-being.
The minimally invasive nature of robotic cancer surgery offers significant advantages for patients. Smaller incisions lead to less scarring, while reduced blood loss minimizes the need for transfusions. This approach not only promotes faster healing but also shortens hospital stays, enhancing overall recovery experiences.
Minimally invasive robotic surgery revolutionizes cancer treatment by utilizing smaller incisions compared to traditional open surgery. This approach significantly reduces trauma to the body, leading to various benefits:
Robotic surgery not only minimizes scarring and accelerates recovery but also significantly reduces blood loss during cancer procedures. Studies indicate that robotic techniques result in considerably less blood loss compared to traditional laparoscopic and open surgeries. For instance, in rectal cancer surgeries, robotic methods demonstrated an average blood loss reduction of 156.63 mL compared to open surgery. This decrease in blood loss translates to a lower need for transfusions, which can enhance overall patient outcomes by minimizing postoperative complications, including infections. Additionally, the precision offered by robotic systems allows surgeons to avoid damaging surrounding tissues, further contributing to reduced blood loss. Consequently, robotic surgery stands out as a beneficial option in cancer care, improving both safety and recovery prospects.
While traditional surgical methods often lead to extended recovery times and longer hospital stays, the advancements in robotic surgery have revolutionized the terrain of cancer treatment. This minimally invasive approach contributes significantly to faster healing and reduced hospital stays. Key benefits include:
Robotic surgery significantly reduces the risk of complications and postoperative side effects, leading to improved patient outcomes. Enhanced sterility during robotic procedures results in lower infection rates, while the minimally invasive approach minimizes postoperative pain and promotes faster recovery. Additionally, patients experience decreased reliance on opioid pain medications, further contributing to a safer and more comfortable recovery process.
Enhanced sterility in surgical procedures plays an essential role in reducing infection rates, particularly in the context of robotic surgery. Studies indicate that robotic surgery leads to significantly lower wound infection rates compared to traditional methods. This is particularly evident in procedures related to prostate and gastric cancers.
Key factors contributing to these lower infection rates include:
These advantages highlight the importance of advanced robotic systems in improving patient outcomes and minimizing postoperative complications.
As surgical techniques continue to evolve, the benefits of robotic surgery in reducing postoperative pain and facilitating faster recovery have become increasingly evident. Studies indicate that patients undergoing robotic procedures experience significantly less postoperative pain compared to traditional laparoscopic surgery, leading to reduced use of patient-controlled analgesia (PCA) and lower total opioid delivery. Robotic surgery also shortens hospital stays by approximately 20%, averaging eight days versus ten for open surgery. In addition, early mobilization and quicker return to daily activities enhance recovery times. With a notable decrease in readmission rates and complications, robotic surgery not only minimizes pain but also promotes a smoother transition back to normal life, establishing a new standard in cancer care.
While the shift towards robotic surgery for cancer care is primarily lauded for its precision and reduced recovery times, it also significantly decreases reliance on opioid pain medications. This decrease is vital for minimizing risks associated with opioid use. Key benefits include:
Such findings highlight the potential for robotic surgery to not only enhance recovery but also encourage better opioid stewardship, ultimately reducing the risk of dependence and associated complications.
Robotic surgery has demonstrated significant advancements in patient outcomes and survival rates, particularly through enhanced surgical precision. By facilitating more effective tumor resections and reducing the risk of cancer recurrence with clearer margins, these procedures contribute to improved long-term prognoses. Consequently, patients often experience a better quality of life following robotic interventions.
Achieving better precision in tumor resection greatly improves patient outcomes and survival rates. Robotic surgery enhances precision through several mechanisms:
These advancements collectively enable more effective tumor resections, ultimately leading to improved survival rates and better overall health for patients.
The reduction of cancer recurrence is significantly influenced by the achievement of clear surgical margins during tumor resections. Robotic surgery enhances precision, allowing surgeons to excise tumors while minimizing damage to surrounding tissues. This precision is vital in attaining clear margins, which are essential for reducing the likelihood of recurrence. Studies indicate that robotic-assisted procedures exhibit lower positive margin rates compared to traditional methods, thereby decreasing the risk of cancer returning. Additionally, robotic surgery has demonstrated comparable long-term oncologic outcomes to laparoscopic approaches, with similar recurrence rates. The ability to achieve clear margins effectively through robotic techniques highlights its role in improving patient outcomes and supports its increasing adoption in cancer treatment protocols.
As advances in surgical techniques continue to evolve, patients undergoing robotic surgery for cancer treatment often experience improved long-term prognosis and enhanced quality of life. This innovative approach offers several key advantages:
These benefits collectively contribute to shorter hospital stays and a quicker return to normal activities, ultimately enhancing the overall quality of life for patients following robotic surgery.
Robotic surgery has revolutionized the treatment of various cancers by offering customized advantages for specific types. For instance, prostate cancer patients benefit from nerve-sparing techniques, while lung cancer surgeries see improvements in tumor resection and safety. Additionally, advancements in robotic surgery enhance precision in colorectal, gynecologic, and head and neck cancer procedures, ultimately leading to better patient outcomes.
While many surgical techniques exist for treating prostate cancer, nerve-sparing robotic prostatectomy has emerged as a preferred option due to its ability to preserve critical neurovascular structures. This minimally invasive approach offers several benefits:
These factors contribute to the growing preference for robotic-assisted prostatectomy in cancer care.
In the domain of cancer treatment, advancements in surgical techniques continue to revolutionize patient care. Robotic surgery for lung cancer offers enhanced precision, allowing surgeons to execute complex resections in confined spaces. The 540-degree rotation of robotic arms facilitates accurate tumor removal and lymph node dissection, while high-definition, 3D visualization improves surgical precision. This minimally invasive approach results in less post-operative discomfort, reduced hospital stays, and lower infection risks. Patients typically recover within 2-3 weeks, returning to daily activities sooner than with traditional methods. The combination of precise tumor resection and reduced morbidity highlights the significant safety benefits robotic surgery provides, ultimately leading to improved outcomes for lung cancer patients.
Advancements in robotic surgery significantly enhance the approach to colorectal cancer treatment, particularly in the area of lymph node dissection. This technique improves cancer staging and patient outcomes through several key benefits:
These advantages contribute to improved overall treatment efficacy, underscoring the role of robotic surgery in colorectal cancer care.
Robotic surgery has revolutionized the treatment of gynecologic cancers, particularly through minimally invasive hysterectomy and staging techniques. This approach employs smaller incisions, resulting in reduced scarring, less postoperative pain, and minimal bleeding. Patients typically experience shorter hospital stays—often just one night—and faster recovery times compared to traditional methods. The precision of robotic surgery, enhanced by 3D imagery and a 360° range of motion, allows surgeons to maneuver complex procedures while minimizing disruption to surrounding tissues. Additionally, this method reduces the risk of complications and infections. Ideal candidates for robotic surgery include patients with early-stage cancers, emphasizing the need for individualized assessments by a specialized surgical team to guarantee optimal outcomes.
While traditional surgical methods often pose challenges in accessing tumors located in the head and neck region, the introduction of robotic surgery has significantly improved surgical access and precision. This innovative approach offers several advantages:
Additionally, transoral robotic surgery (TORS) enables access through the mouth, minimizing external incisions and facilitating tumor treatment in complex locations. These advancements not only enhance surgical outcomes but also prioritize the preservation of essential functions like speech and swallowing, ultimately improving patients’ quality of life.
The comparison between robotic-assisted surgery and traditional open surgery reveals significant differences in precision, recovery time, and complication rates. Additionally, evaluating robotic versus laparoscopic techniques highlights variations in outcomes for cancer patients. Long-term success rates further emphasize the developing environment of surgical options in oncology care.
In comparing robotic-assisted surgery to traditional open surgery, one notable distinction lies in the surgical approach, which significantly impacts patient outcomes. Robotic-assisted surgery employs smaller incisions and advanced technology, leading to various advantages:
These differences contribute to benefits like reduced pain, shorter recovery times, and lower risk of complications, making robotic surgery a persuasive option for cancer care.
How do robotic and laparoscopic surgeries compare in terms of patient outcomes? Robotic surgery generally offers superior results, particularly in complex procedures. For instance, 71% of robotic right colectomies achieved textbook outcomes, compared to 64% for laparoscopic surgeries. Additionally, robotic techniques tend to have lower complication rates, such as fewer conversions to open surgery and reduced instances of postoperative ileus. Enhanced precision and improved lymph node harvesting capabilities further contribute to better cancer staging. While robotic surgery showcases advantages in precision and reduced hospital stays, laparoscopic procedures may still perform comparably in specific cases, such as low anterior resections. Overall, robotic surgery tends to deliver enhanced outcomes in many cancer treatments, though not universally superior in all scenarios.
Robotic surgery is increasingly recognized for its long-term success rates in oncology, particularly when compared to traditional surgical methods. Numerous studies highlight its advantages, which include:
Artificial Intelligence greatly improves the capabilities of surgical robotics by enhancing precision and efficiency in procedures. Through machine learning, these systems can identify and resect tumors with greater accuracy, reducing the risk of damage to surrounding tissues. Additionally, predictive analytics offers personalized understandings that can guide surgeons in tailoring their approach to individual patient needs, ultimately optimizing cancer care outcomes.
In recent years, the integration of artificial intelligence (AI) into surgical robotics has significantly altered the environment of surgical procedures. AI enhances the precision and control of robotic systems, leading to improved surgical outcomes. Key benefits of AI in robotic surgery include:
These advancements not only streamline surgical processes but also contribute to better patient care and recovery in cancer treatments.
As the scenery of surgical practices evolves, machine learning has emerged as an essential tool for enhancing tumor identification and resection during procedures. AI algorithms employ real-time imaging to accurately pinpoint tumor tissue by comparing current images to reference images. These advanced systems can identify anatomical features, tissue margins, and characteristics based on predefined criteria or physician input. With 93% accuracy in specific surgeries, such as robotic prostatectomy, AI enhances precision while minimizing collateral damage. Additionally, AI monitors progress, adjusting surgical plans in real-time, ultimately reducing recovery time and hospital stays. The integration of machine learning not only streamlines surgical processes but also has the potential to revolutionize education and training within the field, ensuring continuous improvement in surgical outcomes.
Predictive analytics plays a vital part in personalizing cancer surgery, enhancing the precision and effectiveness of treatment plans. By integrating varied data sources, predictive analytics supports clinicians in making informed decisions. Key benefits include:
These innovations facilitate targeted interventions and improve overall patient outcomes, demonstrating the significant potential of predictive analytics in robotic cancer surgery.
The future of robotic surgery in cancer care promises significant advancements in technology and accessibility. Innovations such as miniaturization and AI integration are set to enhance surgical precision and expand treatment options for various cancers. As access to robotic surgery increases, more patients will benefit from these advanced techniques, ultimately revolutionizing oncology treatment.
While advancements in robotic-assisted surgical technology continue to reshape cancer care, the integration of enhanced precision, reduced complications, and innovative techniques stands at the forefront of this change. Key innovations include:
These advancements not only improve surgical outcomes but also enhance surgeons’ skills, ultimately benefiting patient care and recovery in the field of cancer treatment.
As advancements in robotic surgery continue to emerge, expanding access to these innovative techniques becomes essential for enhancing cancer care across varied populations. Key partnerships between hospitals, research institutions, and technology companies are vital for deploying robotic systems in rural areas, addressing disparities in access to skilled surgeons. Initiatives like the SARRTS project at Children’s National Hospital enable general surgeons in remote settings to employ robotic technology for complex procedures. Enhanced training opportunities through remote demonstrations and simulation-based programs allow surgeons to adapt to new techniques effectively. Additionally, single-port robotic systems minimize tissue impact and improve patient outcomes. By increasing accessibility to specialized surgical care, robotic surgery promises earlier interventions and better results for a broader range of patients.
Robotic surgery is set to revolutionize oncology treatment, offering innovative solutions that enhance precision and minimize invasiveness. This next generation of surgical techniques promises significant advancements in cancer care, including:
With these advancements, robotic surgery not only improves patient outcomes but also encourages ongoing innovation, ensuring that cancer treatment continues to evolve and adapt to the needs of patients in the future.
Given the advancements in surgical technology, robotic surgery has emerged as a revolutionary approach in cancer care. This innovative technique offers enhanced precision and accuracy, allowing for better access to difficult tumors and improved surgical outcomes. Patients benefit significantly from reduced recovery times, less pain, and lower rates of complications, all due to minimally invasive procedures. In addition, robotic surgery enhances the surgeon’s ability to perform complex tasks with greater dexterity and control.
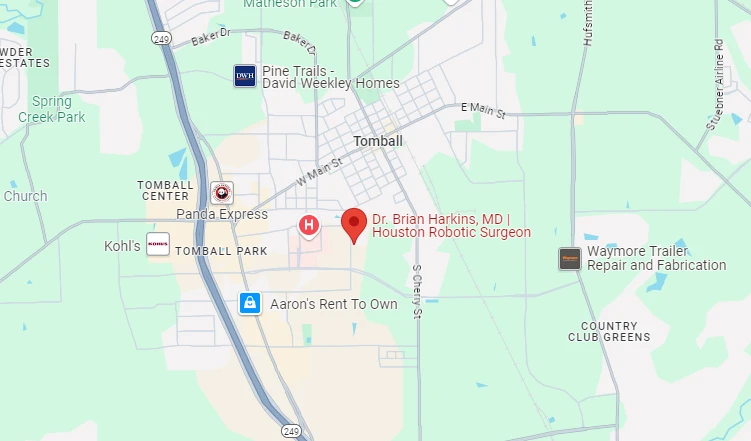
As ongoing innovations continue to evolve in this field, the integration of robotic surgery with other treatment modalities promises to further improve patient care. At Dr. Brian Harkins’ practice, we are committed to leading the way in advanced robotic-assisted surgery, ensuring that our patients receive the most effective, precise, and minimally invasive cancer treatments available today.
The adoption of robotic surgery has significantly enhanced the precision and effectiveness of surgical techniques, particularly in oncology. Robot-assisted surgery, also known as robot-assisted surgery, enables surgeons to perform complex procedures with greater accuracy and control than conventional laparoscopic surgery. This robotic approach has improved outcomes for patients with prostate cancer, endometrial cancer, and rectal cancer, making it a standard of care in many leading cancer centers worldwide.
The benefits of minimally invasive surgery include smaller incisions, reduced blood loss, shorter hospital stays, and faster recovery times. Unlike open surgery, which requires larger incisions and longer recovery periods, robotic surgical systems and robotic-assisted laparoscopic surgery offer patients less pain and fewer postoperative complications. Studies have shown that robotic surgery can reduce surgical trauma while maintaining high precision and better oncologic outcomes.
Robotic surgery in gynecologic oncology has revolutionized procedures such as staging for endometrial cancer and patients undergoing robotic hysterectomy. The use of robotic surgery allows for minimally invasive techniques that reduce the need for laparotomy for endometrial cancer, resulting in shorter recovery times and improved patient comfort. Surgeons use robotic platforms like the da Vinci robotic surgical system to perform delicate procedures with enhanced visualization and precision.
Recent advancements in robotic technology have led to significant improvements in robotic surgical systems. The introduction of the robotic platform has expanded its applications beyond oncology to cardiac surgery, thoracic surgery, and urological surgery. Emerging surgical robotic technology continues to refine precision and reduce complications, making robotic surgery a preferred option for many complex procedures.
While both laparoscopic and robotic procedures are minimally invasive, the robotic approach provides greater flexibility, enhanced dexterity, and improved visualization. Conventional laparoscopic surgery relies on rigid instruments, whereas robot-assisted laparoscopic surgery allows for wristed instruments that mimic natural hand movements, leading to better surgical outcomes. Studies show that robotic surgery may improve patient safety and reduce conversion rates to open surgery in complex cases.
As robotic surgery is still evolving, maintaining oversight in robotic surgery is crucial to ensuring patient safety and procedural success. Institutions and regulatory bodies monitor the cost-effectiveness of robotic surgery, training programs, and outcomes to improve the acceptance of robotic surgery. Additionally, with telesurgery or remote surgery becoming more prevalent, proper guidelines and safety measures are necessary to prevent complications.
Robotic-assisted surgery has extended its applications beyond oncology to general surgery and urological surgery. In patients with prostate cancer, the use of robotic platforms enhances precision during prostatectomy, leading to improved functional outcomes. Similarly, in resection for rectal cancer, robotic technology facilitates better access to deep pelvic structures, reducing the need for conversion to open surgery.
The cost-effectiveness of robotic surgery remains a topic of debate as hospitals weigh the benefits of improved patient outcomes against the initial investment in robotic surgical platforms. While robotic procedures can be more expensive than conventional laparoscopic or open surgery, studies suggest that robotic surgery is associated with shorter hospital stays, fewer complications, and reduced long-term healthcare costs. These factors contribute to the growing acceptance of robotic surgery across various medical specialties.
The history of robotic surgery dates back to early developments in surgical robotic technology. The current state of robotic surgery is a result of decades of research, innovation, and refinement. The development in robotic-assisted surgery has led to robotic platforms like the da Vinci robotic surgical system, which has become the leading robotic approach in modern surgery. As technology advances, robotic surgery continues to evolve, providing better patient outcomes and improved procedural accuracy.
The future of robotic surgery in the treatment of cancer looks promising, with advancements in robotic technology continuing to improve patient outcomes. Researchers are exploring new applications in robotic surgery, including AI-assisted navigation and real-time imaging. Surgery with da Vinci and other robotic surgical systems is expected to expand, making robotic-assisted surgical techniques more accessible and effective. As a leader in robotic surgery, many institutions are integrating these technologies into routine practice to provide safer, more precise cancer treatments.

Dr. Brian Harkins is a renowned surgeon specializing in advanced, minimally invasive, and robotic surgical techniques. With a dedication to innovation and personalized patient care, he has transformed countless lives by delivering exceptional outcomes.
I want a website like this, where do i start?