
Multi-modal pain management greatly improves postoperative recovery in robotic and minimally invasive surgeries. It integrates various analgesic therapies, reducing reliance on opioids while promoting effective pain relief. This approach combines non-opioid analgesics, regional anesthesia, and anti-inflammatory medications to optimize healing. As a result, patients experience shorter hospital stays and improved mobility, which are essential for recovery. Exploring this strategy further reveals its potential and broader implications for modern surgical practices.
Pain management in robotic and minimally invasive surgeries represents a significant evolution in surgical practices. Traditional methods often fall short, leading to inadequate pain control that can adversely affect postoperative recovery. The precision and reduced invasiveness of these modern techniques not only influence pain levels but also contribute to improved outcomes for patients. Moreover, the use of robotic systems enhances surgical precision during operations, which can lead to a reduction in postoperative pain and complications.
As surgical techniques have evolved, the focus on pain management has shifted significantly, particularly with the rise of robotic and minimally invasive surgeries. Multi-modal pain management in surgery addresses the unique challenges posed by these advanced techniques, emphasizing strategies that reduce postoperative pain. Minimally invasive surgery pain relief is achieved through smaller incisions and less tissue trauma, leading to quicker recovery times and decreased reliance on strong pain medications. Enhanced precision provided by robotic systems minimizes complications, further improving postoperative pain control strategies. As a result, patients experience shorter hospital stays, fewer risks of infections, and an overall enhanced quality of life, marking a significant advancement in the evolution of surgical pain management. The implementation of robotic surgery has allowed for even greater advancements in pain management techniques, ensuring that patients benefit from the latest surgical innovations.
While traditional pain management methods have served as the foundation for postoperative care, they often fall short in the structure of robotic and minimally invasive surgeries. These approaches frequently rely on opioids, which carry a significant risk of addiction and may not provide long-term relief. Additionally, traditional methods typically lack the personalized care necessary for effective pain management after robotic surgery, often disregarding individual patient needs. In contrast, the adoption of opioid-free pain management techniques and a multi-modal pain relief protocol can lead to better outcomes. By addressing the limitations of conventional methods, healthcare providers can enhance recovery while minimizing complications associated with inadequate pain control, ultimately leading to a more effective and patient-centered postoperative experience. The Eighth World Congress of Laparoscopic Surgeons emphasizes the importance of improving surgical outcomes for patients, which includes effective pain management strategies.
Effective pain control is essential for optimal postoperative recovery, especially in the context of robotic and minimally invasive surgeries. Poor pain management can lead to delayed recovery, impaired physical function, and increased risk of complications such as severe vein thrombosis. The psychological impact is significant, with high pain levels contributing to anxiety, depression, and cognitive impairment. In addition, inadequate pain relief raises the risk of chronic pain, particularly when comparing regional anesthesia vs opioid pain relief strategies. Enhancing recovery with multi-modal pain management approaches can mitigate these issues, improving overall patient outcomes and reducing healthcare costs. Ultimately, effective postoperative pain management not only aids recovery but also minimizes the long-term ramifications of poorly controlled pain.
Robotic and minimally invasive surgical techniques significantly influence pain levels experienced by patients postoperatively. Smaller incisions created by these methods lead to less trauma, reducing muscle and nerve disruption, and ultimately alleviating pain. This precision also allows for effective non-opioid pain control after surgery, minimizing the need for pain medication and its associated side effects. Enhanced visualization provided by robotic systems enables surgeons to operate with greater accuracy, resulting in fewer complications and decreased postoperative inflammation. Consequently, patients experience faster recoveries, shorter hospital stays, and an improved quality of life. A multi-disciplinary approach to surgical pain relief further enhances these benefits, ensuring thorough management of pain and facilitating quicker returns to normal activities.
Multi-modal pain management is an approach that integrates various analgesic therapies to provide extensive pain relief. By leveraging medications with distinct mechanisms of action, it targets pain pathways effectively while minimizing opioid use. This strategy not only enhances patient outcomes but also contrasts sharply with traditional opioid-only protocols.
A thorough approach to pain management involves the use of multiple strategies that target different pathways of pain relief. Multi-modal pain management combines various medications and interventions to optimize post-surgical recovery pain management. Key components include non-opioids like acetaminophen and NSAIDs, alongside local techniques such as nerve blocks for post-surgery pain control. This strategy aims to minimize opioid reliance while enhancing overall pain relief. Studies indicate that employing the best pain management strategies for robotic surgery can significantly improve patient outcomes and reduce side effects. By integrating these varied methods, healthcare providers can create individualized protocols that effectively address pain while promoting faster recovery and better quality of life for patients post-surgery.
While pain management in surgical settings has traditionally relied heavily on opioids, a more refined approach known as multi-modal pain management has emerged. This strategy combines different classes of medications—such as local anesthetics, NSAIDs, and acetaminophen—to address the unique and variable nature of pain. The science behind this approach lies in its ability to provide synergistic effects, enhancing pain relief while minimizing opioid dependence and side effects. By utilizing customized combinations of drugs, healthcare providers can support early mobilization in pain recovery, facilitating quicker rehabilitation and improved patient experiences. The adaptability and effectiveness of multi-modal pain management make it a vital component in modern postoperative care.
When comparing multi-modal pain management to opioid-only protocols, it becomes evident that the former offers a more comprehensive approach to addressing postoperative pain. Multi-modal pain management (MMA) enhances pain control by integrating non-opioid analgesics, which significantly reduces opioid consumption and associated side effects like nausea and constipation. This method not only results in lower pain scores but also promotes quicker recovery times and improved mobilization post-surgery. Additionally, the all-encompassing nature of MMA addresses both psychological and physiological aspects of pain, potentially leading to fewer complications and lower readmission rates. Current guidelines advocate for combining opioids with non-opioid therapies and tapering opioid use to minimize dependency, further underscoring the advantages of MMA over traditional opioid-only protocols.
Key components of multi-modal pain management include a variety of strategies aimed at enhancing pain relief while minimizing opioid use. Non-opioid analgesics, regional anesthesia, and anti-inflammatory medications play vital roles in addressing different aspects of pain, while physical therapy and psychological support contribute to overall recovery. By integrating these approaches, healthcare providers can create a thorough pain management plan customized to individual patient needs.
Non-opioid analgesics play an essential role in the multi-modal approach to pain management, particularly in surgical settings. These medications, including non-steroidal anti-inflammatory drugs (NSAIDs) and agents like duloxetine, are effective in reducing pain while minimizing reliance on opioids. However, their use requires careful consideration. Patients at high risk for gastrointestinal side effects or renal damage, such as the elderly or those with a history of peptic ulcers, should use NSAIDs cautiously. Additionally, the concomitant use of these analgesics with anticoagulants can increase the risk of bleeding. It is also advisable to taper these medications gradually when discontinuing to avoid withdrawal symptoms, ensuring a safer and more effective postoperative recovery.
The integration of regional anesthesia and nerve blocks greatly improves the effectiveness of multi-modal pain management strategies in surgical settings. These techniques provide targeted pain relief, significantly reducing discomfort during and after procedures. By minimizing the need for intravenous opioids, nerve blocks not only enhance patient satisfaction but also lower the risk of opioid addiction. Various types of blocks, such as femoral and adductor canal blocks, cater to specific surgical needs, offering both safety and efficacy when administered by trained professionals. Utilizing ultrasound guidance guarantees precise medication delivery, prolonging pain relief for hours to days. Overall, regional anesthesia and nerve blocks play an essential role in facilitating quicker recovery and improved postoperative outcomes in patients undergoing robotic and minimally invasive surgeries.
Anti-inflammatory medications, particularly nonsteroidal anti-inflammatory drugs (NSAIDs), play an essential role in managing postoperative pain by effectively reducing swelling and discomfort. Commonly used NSAIDs, such as ibuprofen and naproxen, work by inhibiting the cyclooxygenase pathways, thereby decreasing inflammation and alleviating pain. This dual action not only enhances patient satisfaction but also minimizes the need for opioids, reducing associated side effects. While NSAIDs are generally safe, they do carry risks, including gastrointestinal bleeding and renal dysfunction, particularly in sensitive populations. Selective COX-2 inhibitors like celecoxib offer a safer alternative, targeting inflammation without the gastrointestinal risks. Overall, incorporating NSAIDs into multimodal pain management strategies can significantly improve recovery outcomes following surgery.
Effective physical therapy and early mobilization are vital components of a successful postoperative recovery strategy. These practices significantly reduce the risk of complications and accelerate the recovery of functional walking capacity. Additionally, early mobilization enhances patient-reported outcomes by alleviating pain and fatigue while improving overall quality of life. It is associated with shorter hospital stays, thereby reducing healthcare costs. Successful early mobilization relies on preoperative education, structured protocols, and supervised exercises to improve patient engagement and compliance. A multidisciplinary approach, involving healthcare professionals from various fields, is essential for effective implementation. By enabling patients to actively participate in their recovery, early mobilization cultivates a culture of physical activity that benefits long-term health outcomes.
Integrating psychological support into pain perception management is essential for enhancing postoperative recovery outcomes. Psychological factors such as anxiety and depression significantly predict both acute and chronic post-surgical pain. Young patients and those with preoperative pain or emotional distress are particularly vulnerable. Interventions like Cognitive Behavioral Therapy (CBT) effectively address negative beliefs and coping strategies, promoting better pain management and functional recovery. Additionally, psychoeducation and relaxation therapy can help patients alter their pain perception. Positive psychological traits, such as optimism and self-efficacy, serve as protective factors against pain. By addressing psychological aspects alongside physical care, healthcare providers can improve overall recovery experiences for patients undergoing robotic and minimally invasive surgeries.
Multi-modal pain management in postoperative recovery offers significant advantages, including faster recovery times and reduced hospital stays. By minimizing opioid dependence and associated side effects, patients experience improved mobility and rehabilitation outcomes. Ultimately, these strategies enhance patient satisfaction and quality of life following surgery.
While traditional pain management often relies heavily on opioids, recent advancements in postoperative care emphasize the importance of combining various analgesic strategies to enhance recovery. Multi-modal pain management, which includes the use of non-opioid medications and local infiltration techniques, significantly reduces the need for high-dose opioids. This approach not only alleviates pain effectively but also encourages early mobilization, critical for minimizing hospital stays. Implementing Enhanced Recovery After Surgery (ERAS) protocols further standardizes these strategies, leading to shorter hospitalizations and improved patient outcomes. By decreasing opioid consumption and associated side effects, multi-modal analgesia promotes a smoother recovery, allowing patients to return to their daily activities more quickly, ultimately benefiting both healthcare systems and individuals.
As postoperative care evolves, the adoption of multi-modal pain management strategies significantly mitigates the risks associated with opioid dependence and side effects. By reducing opioid consumption through the use of non-opioid analgesics and targeted local anesthetic blocks, patients undergoing robotic surgeries may often be discharged without opioid prescriptions. This approach not only decreases the likelihood of opioid-related complications but also minimizes respiratory risks, evidenced by a notable reduction in respiratory complications among hip replacement patients. Additionally, the combination of various analgesics enhances pain control while limiting opioid use, nurturing improved recovery outcomes. Overall, multi-modal pain management stands as a powerful tool in improving postoperative care, reducing opioid reliance, and encouraging safer recovery experiences.
Effective pain management strategies significantly enhance patient mobility and rehabilitation outcomes after surgery. Multimodal pain management techniques, including epidural analgesia and peripheral nerve blocks, minimize opioid usage, which helps patients recover bowel function more quickly and reduces side effects that impair movement and energy levels. These protocols facilitate early mobilization, essential for preventing complications such as profound vein thrombosis. Additionally, the integration of medications like gabapentin and intravenous lidocaine has been shown to lower pain scores and improve postoperative mobilization. Enhanced Recovery After Surgery (ERAS) protocols further emphasize these strategies, leading to improved patient experiences and quicker rehabilitation. Overall, optimized pain control nurtures a smoother recovery pathway and promotes better long-term outcomes for surgical patients.
Multi-modal pain management not only enhances patient mobility and rehabilitation outcomes but also significantly contributes to overall patient satisfaction and quality of life following surgery. By reducing opioid use, this approach minimizes side effects and complications, leading to better pain control and quicker recovery. Patients benefit from standardized protocols that encourage early mobilization, which is essential for long-term pain management. Additionally, a comprehensive approach addressing both physical and psychological aspects of pain results in decreased anxiety and improved mood. As a result, patients experience shorter hospital stays and a faster return to normal activities. Ultimately, the combination of effective pain management and reduced reliance on opioids enhances the overall patient experience and satisfaction post-surgery.
Implementing multi-modal pain management in surgical protocols requires thorough preoperative planning to guarantee optimal pain control. Intraoperative techniques that minimize postoperative discomfort must also be integrated, along with effective strategies for long-term pain management. Additionally, the development of personalized pain management plans is essential to address the unique needs of each patient.
While preoperative planning is often overlooked, it plays an essential role in optimizing pain control during surgical procedures. Extensive pain and medication assessments are critical, involving a detailed review of analgesic use, including opioids, and psychosocial factors. For patients with complex pain needs, customized post-anesthesia care plans are necessary. Preoperative counseling can alleviate anxiety and clarify expectations regarding pain management, while opioid-sparing strategies should be integrated into the plan. Collaboration among multidisciplinary teams enhances recovery, ensuring that preoperative medical care and analgesic strategies are standardized. Routine use of local and regional anesthesia, along with regular administration of basic analgesics, can significantly improve postoperative outcomes, aligning with evidence-based practices in multi-modal pain management.
Effective pain management strategies during surgery significantly impact postoperative recovery. Intraoperative techniques such as local infiltration of liposomal bupivacaine (Exparel) provide effective pain control, offering up to 72 hours of relief. Its use is guided by specific protocols for various surgeries, including total knee arthroplasties. Additionally, intravenous nonsteroidal anti-inflammatory drugs (NSAIDs) like meloxicam reduce postoperative pain and decrease opioid reliance. Ultrasound-guided regional blocks, such as interscalene and IPACK blocks, target specific nerves for effective analgesia while minimizing complications. A multimodal approach, integrating these methods, not only optimizes pain control but also aligns with enhanced recovery after surgery (ERAS) protocols, ultimately leading to improved surgical outcomes and reduced morbidity.
A thorough approach to postoperative pain management is essential for ensuring long-term relief and enhancing recovery outcomes. Implementing a multi-modal strategy, which includes scheduled administration of non-opioid medications like NSAIDs, acetaminophen, and local anesthetics, is vital. These methods can significantly improve pain control while reducing reliance on opioids. In addition, employing regional anesthetics and ketamine can additionally decrease opioid consumption and enhance analgesia. Continuous monitoring of the patient’s response allows for timely adjustments, ensuring optimal pain management. Moreover, incorporating non-pharmacological interventions and educating patients and caregivers promotes cooperation, leading to more effective outcomes. By prioritizing these strategies, healthcare providers can improve patient satisfaction, reduce chronic pain risks, and facilitate quicker recoveries.
Personalized pain management plans play an essential role in enhancing surgical outcomes and patient satisfaction. These plans are developed through thorough preoperative assessments that consider genetic variations, histories of chronic pain, psychological factors, and existing health conditions. By evaluating pain sensitivity, healthcare providers can predict how patients will respond to different medications. Implementing multi-modal strategies, such as utilizing non-opioid medications, regional anesthesia, and adjuvant drugs, further tailors pain management to individual needs. Additionally, advancements in AI-driven monitoring allow for real-time adjustments based on patient feedback, ensuring that interventions are both effective and timely. This personalized approach not only optimizes pain relief but also minimizes reliance on opioids, promoting safer recovery pathways for patients.
Future trends in multi-modal pain management for surgical recovery are increasingly shaped by innovations in non-opioid pain medications and data-driven approaches utilizing artificial intelligence. The integration of patient monitoring and wearable technology enhances real-time assessments, allowing for customized interventions. Additionally, multi-disciplinary approaches promise to improve outcomes by combining various treatment modalities to address pain more effectively.
As the terrain of surgical recovery evolves, innovations in non-opioid pain medications are emerging as critical components of multi-modal pain management strategies. Non-steroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen and naproxen effectively alleviate pain by blocking COX enzymes, while acetaminophen raises the pain threshold without anti-inflammatory effects. Combining these medications enhances pain relief and reduces the need for opioids. Additionally, long-acting local anesthetics like EXPAREL provide targeted pain control, minimizing systemic side effects. Recent advancements in drug delivery systems and personalized medicine further optimize pain management approaches. By integrating these innovative non-opioid options, healthcare providers can facilitate faster recovery times and significantly lower opioid consumption in postoperative patients.
The integration of artificial intelligence (AI) and data-driven approaches is reshaping pain management strategies in surgical recovery. AI models can predict which patients might require additional opioid refills by analyzing factors such as surgery type and patient-reported pain levels. For instance, knee replacement surgery is notably linked to increased opioid needs. These predictive models enable physicians to identify at-risk patients, allowing for the development of alternative pain control strategies that reduce dependency on opioids. Personalized pain management takes this further by utilizing patient data and preoperative pain profiling to customize treatment plans. This method not only enhances recovery outcomes but also shortens hospital stays, demonstrating the significant potential of AI in improving postoperative pain management.
Patient monitoring and wearable technology are becoming essential components in the evolution of multi-modal pain management for surgical recovery. These devices track crucial signs preoperatively, facilitating baseline data collection and risk assessment while improving patient compliance with medication and exercise routines. During surgery, real-time data access enhances communication among the surgical team, allowing for immediate adjustments and reducing human error. Postoperatively, wearables continuously monitor recovery metrics, aiding in the early detection of complications and promoting personalized rehabilitation programs. Research indicates that patients using wearables engage in more vigorous activities and experience better physical function. As technology advances, wearables hold promise for optimizing postoperative care and potentially reducing rehospitalization rates through proactive monitoring and intervention.
Advancements in technology, such as patient monitoring and wearable devices, have laid the foundation for integrating multi-disciplinary approaches in pain management. The implementation of multimodal analgesia combines various strategies, including pharmacologic methods and non-pharmacologic techniques like acupuncture and cryotherapy. This collaborative structure, involving anesthesiologists, surgeons, and other healthcare professionals, enhances postoperative recovery by optimizing pain relief and reducing reliance on opioids. Innovations in drug delivery systems, including localized pain relief devices and autoPCA+ systems, further streamline patient care. Digital health technologies facilitate personalized pain management strategies, while AI-driven analytics predict pain outcomes, enabling proactive interventions. This thorough integration of disciplines and technologies sets the stage for improved patient outcomes in surgical recovery.
Effective pain management is a cornerstone of successful surgical outcomes. Multi-modal analgesia (MMA) considerably improves postoperative recovery by integrating various analgesic medications to provide superior pain control while minimizing opioid use. This all-encompassing approach not only addresses multiple pain pathways but also reduces the risk of adverse effects associated with higher opioid consumption. As a key element of Enhanced Recovery After Surgery (ERAS) protocols, MMA promotes faster mobilization and diminishes complications such as nausea and sedation. In addition, effective pain control is linked to improved long-term outcomes, including reduced chronic pain syndromes and lower readmission rates. At Dr. Brian Harkins, we prioritize continuous evaluation and customized pain management strategies to ensure optimal patient care, reinforcing the vital role of multi-modal pain management in modern surgical practices.
Effective acute postoperative pain management requires a multimodal analgesic approach that combines different pharmacologic and non-pharmacologic interventions. According to a systematic review of randomized controlled trials, incorporating non-opioid analgesics reduces postoperative opioid use and improves postoperative analgesia while minimizing side effects. Following practice guidelines for acute pain, this approach is widely recommended for pain management in the perioperative setting.
A randomized controlled trial published in J Pain Res found that a multimodal analgesic regimen significantly reduces postoperative opioid use in patients undergoing laparoscopic colorectal surgery. By targeting different pain pathways, multimodal therapies lower opioid requirement, enhance analgesic efficacy, and improve overall management of postoperative pain in surgery patients.
The transversus abdominis plane block is a regional anesthesia technique proven effective in managing postsurgical pain in patients undergoing laparoscopic and abdominal surgery. Studies, including those in Br J Anaesth, show that TAP blocks significantly reduce postoperative opioid use, improve postoperative pain score, and decrease length of stay following major surgery.
Pain management after laparoscopic colorectal surgery relies on multimodal techniques to address visceral pain, improve perioperative pain control, and minimize complications. A systematic review of multimodal approaches in patients undergoing colorectal surgery showed reductions in postoperative opioid use, better pain relief, and fewer postoperative complications.
According to a double-blind randomized controlled trial, effective acute pain management contributes to faster recovery by reducing postoperative complications, improving pain in patients undergoing surgery, and decreasing opioid-related side effects. Implementing a management of acute postoperative pain strategy ensures better outcomes, particularly in colon and rectal surgery patients.
Compared to open procedures, laparoscopic surgeries are associated with reduced postoperative pain following surgery. However, patients still experience acute postoperative pain following surgery, requiring a well-structured pain management in patients undergoing laparoscopic procedures. A review of randomized controlled trials highlights that multimodal strategies effectively reduce postoperative opioid needs while enhancing analgesia for patients undergoing minimally invasive procedures.
The implementation of enhanced recovery protocols focuses on early mobilization, optimized nutrition, and improved pain management in the perioperative phase. According to J Pain, integrating multimodal strategies within enhanced recovery pathways reduces postoperative day pain scores, accelerates healing, and decreases postoperative period complications.
The task force on acute pain recommends a multimodal approach for pain management in patients following surgery. These guidelines for acute pain management emphasize reducing postoperative opioid dependence, improving management after laparoscopic colorectal surgery, and ensuring early mobilization to prevent complications.
Recent studies in Pain Med and J Pain Res suggest that implementing multimodal approaches in patients undergoing laparoscopic and colorectal surgeries can significantly lower opioid use among patients. Techniques such as regional anesthesia, NSAIDs, and acetaminophen-based protocols enhance postoperative analgesic effects while reducing reliance on opioids.
A systematic review found that multimodal therapies in patients undergoing laparoscopic colorectal surgery lead to reduced postoperative pain after laparoscopic surgery, improved management of postoperative pain, and shorter hospital stays. Pain management after laparoscopic colorectal procedures benefits significantly from multimodal approaches that optimize pain relief while ensuring less opioid consumption.
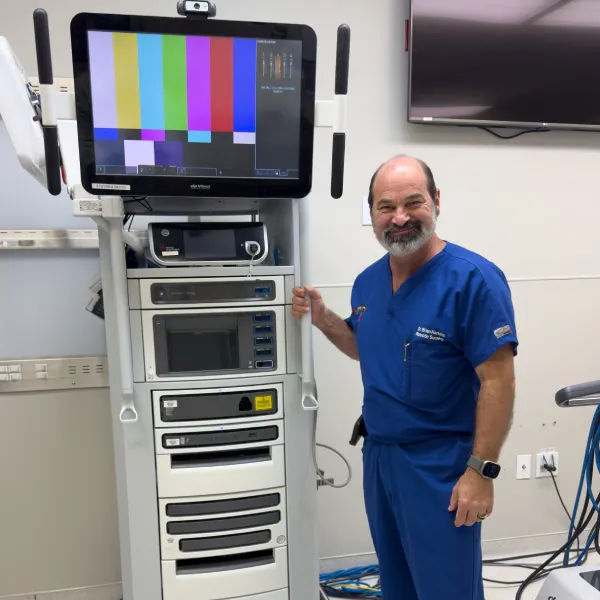


Dr. Brian Harkins is a renowned surgeon specializing in advanced, minimally invasive, and robotic surgical techniques. With a dedication to innovation and personalized patient care, he has transformed countless lives by delivering exceptional outcomes.

I want a website like this, where do i start?